Episode 95:
Navigating Medicare Audits and Appeals
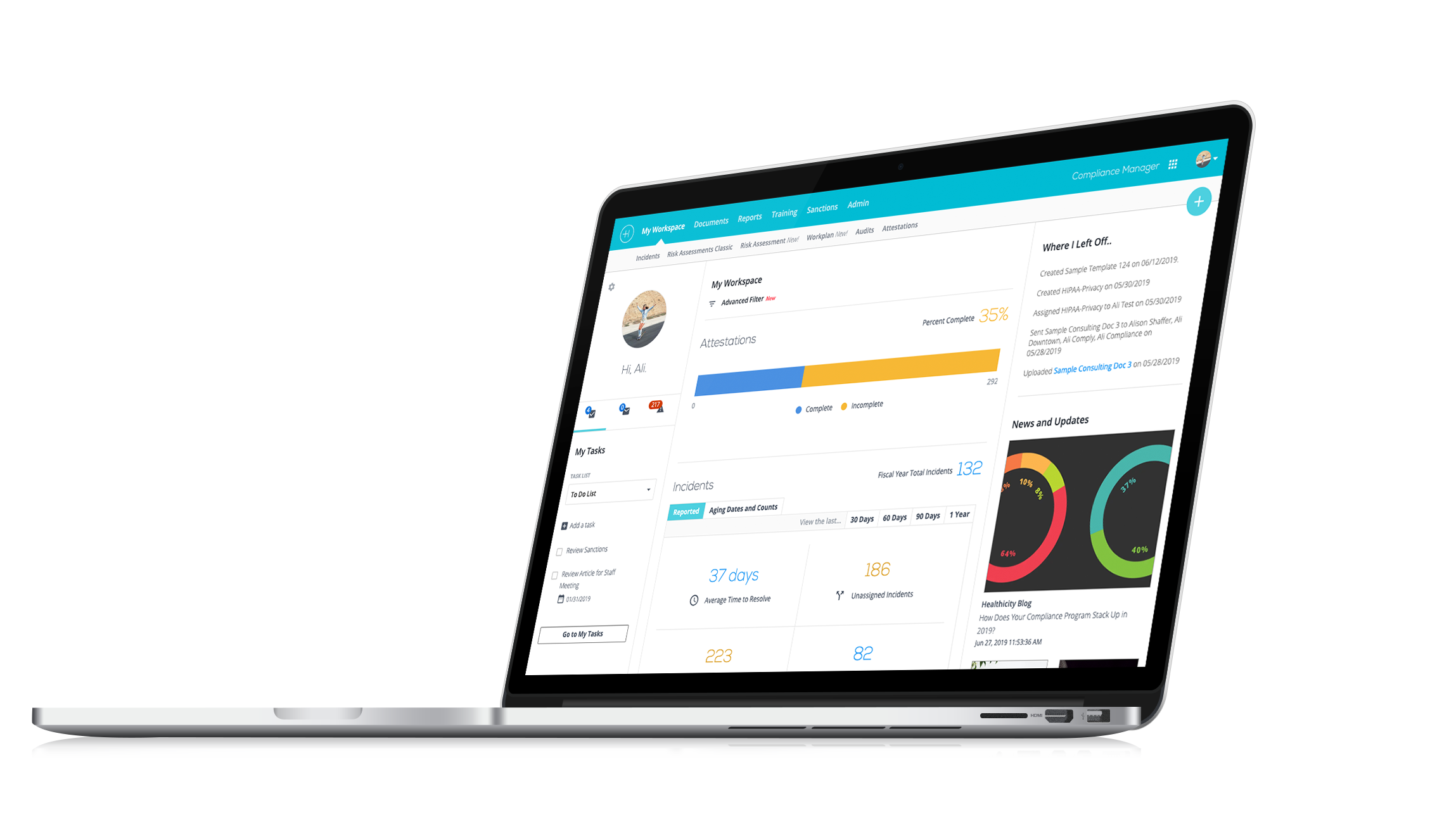
Watch the demo:
Compliance Manager
See the only all-in-one compliance solution today.
Is your practice audit-ready? Get the expert insights you need to navigate Medicare audits smoothly.
Medicare audits can be a daunting challenge for any healthcare provider. With a maze of regulations, different types of audits, and a complex appeal process, it’s easy to feel overwhelmed.
That’s why we invited Alicia Shickle, AHFI, CHC, CPC, CPCO, CPMA, CRC, the President and CEO of ProCode Compliance Solutions LLC, to share the knowledge and strategies you need to navigate this tricky terrain.
Tune in to the episode as we discuss:
- Some of the top issues that trigger Medicare audits
- How to prepare your practice and avoid common pitfalls
- The five levels of Medicare appeals and how to effectively manage them
- Why proactive compliance programs are crucial for your practice
Thank you, Alicia, for sharing your time and expertise with us!
About Alicia Shickle
Alicia has decades of clinical and administrative healthcare experience. Her areas of expertise include revenue cycle integrity, documentation, coding and billing compliance, Medicare, MSP, and Medicaid regulations, practice workflow and operations, compliance program assessments, development, and implementation.
Alicia provides advisory services to attorneys, healthcare administrators, providers, and organizations. She frequently works with business litigation and health law practices on fraud and abuse intervention and providing independent and objective assessments for both plaintiff’s and defense teams.
She works closely with clients on both routine and complex documentation and coding reviews. She provides in-depth coding and claims data analysis, education, and assists providers with navigating complex regulatory and policy requirements, identifying and mitigating potential FCA risks while optimizing revenue. She has extensive experience developing and implementing effective compliance programs including all seven elements.
Alicia served as the Director of Compliance for the American Academy of Professional Coders (AAPC). She has worked with some of the top consulting and health law practices and, was a Family Practice Administrator for over a decade.
Alicia has presented educational training boot camps and seminars nationally on compliance, documentation and coding, and practice management. She was a medical billing and coding instructor at a community college. She is a frequent author for online physician blogs, and journals. Alicia is an Accredited Health Care Fraud Investigator (AHFI) with the National Health Care Anti-Fraud Association (NHCAA), and is certified in Healthcare Compliance (CHC, CPCO) through the Health Care Compliance Association (HCCA), and AAPC. She is a Certified Professional Coder (CPC), Certified Professional Medical Auditor (CPMA), and certified in Risk Adjustment Coding (CRC). She is also a Certified Physician Practice Manager (CPPM).
Alicia is an active member of the American Academy of Professional Coders (AAPC) and served as the President of AAPC’s Manhattan Local Chapter for two years. She is a member of the Health Care Compliance Association (HCCA), and the National Health Care Anti-Fraud Association (NHCAA), and American Health Lawyers Association (AHLA). She is a member of American Health Information Management Association (AHIMA), the National Alliance of Medical Auditing Specialists (NAMAS), and a member of Medical Group Management Association (MGMA).
Interested in being a guest on the show? Email CJ directly here.
Episode Transcript
CJ: Welcome everybody to another episode of Compliance Conversations. My name is CJ Wolf with Healthicity and we have another wonderful topic today. We are going to be talking about audits and Medicare audits and appeals and all those kinds of fun things. And our guest is Alicia Shickle. Welcome to the podcast, Alicia.
Alicia: Hi, thank you for having me.
CJ: Yeah, we're excited everybody. Alicia's got so much experience in this area. So, I'm really excited to kind of get into this topic. But before we do that, Alicia, we'd love to hear a little bit more about you, you know, maybe a little bit about your background or your current work or whatever you feel comfortable sharing.
Alicia: Oh boy! Awesome! Well, thank you! I really appreciate it. I think today's topic is so important to kind of get out there and talk to folks about, you know, I don't know. It kills me every time I say it, but I've been in the industry almost 40 years, right? Four decades, I know. I'm always like, it's a shocker when I say it out loud.
CJ: Right!
Alicia: I started out in clinical many, many moons ago and I moved into administration, so I was a family practice administrator for over a decade. I worked with many providers in my area on coding. I got certified in coding when I became an administrator, just so that I could really have a good handle on my own revenue cycle and I loved it and a lot of docs in the area started reaching out to me, you know, and then I really became very proficient in revenue cycle and compliance. We took our practice to be like the first Level 3 accredited NCQA practice in the state of New York for getting on an EMR. Yeah, it was super, super exciting. I have been working in a consulting capacity a 100% for like the last probably 15 years providing education, helping docs, you know, develop compliance and implement compliance programs, revenue cycle integrity. So, it's been a journey. It's always evolving which you know we want to absolutely we always teach our clients and you know make sure everyone knows that you know the only constant thing in healthcare is change so that's critical to keep up with everything.
CJ: Yeah, that's so true. And I actually kind of enjoy that change. It's kind of what keeps things interesting. But you're absolutely right and you know, maybe we'll include if you're comfortable, at least we can include a link to your consulting website or your LinkedIn or however you want to share that. So, if people listening would like to reach out to Alicia professionally, you will have that opportunity.
Alicia: Thank you! Sure!
CJ: Awesome! Well, Alicia, let's jump in. You know, because you and I have known each other for a little while. So, I've known, you know, kind of the breadth and the vast experience that you have with clients. And that's really what I was hoping we could talk about today, and because you see clients all over the country, and I know you're probably seeing all sorts of like Medicare audits and appeals and so maybe we could just kind of start with what are the top four or five issues that you see on a regular basis or you know amongst all the clients that you're working with around the country?
Alicia: Yeah, absolutely! You know, and it's important to kind of understand I think just kind of you know, coming out of the gate that there are different types of Medicare audits, right? We have, you know, target proven educate audits, those are audits that are conducted by the MACs. Mostly those types of audits and they are basically what they say they are right. Providers are like targeted analytically, they're probed, which is their audit piece, you know, and then they're educated. So, those types of audits we see quite frequently, they pretty much focus on like medical necessity for specific issues or outlier providers, we also do a lot of work with providers who are under what they call UPIC audits. Those are unified program integrity contractor reviews. Those UPIC auditors are really looking more for like fraud, waste, abuse issues. We see those audits are more statistically valid random samples. They apply extrapolations which we can talk a little bit about. And then we're seeing, you know, SMRC audits and RAC audits. Some of the biggest issues that we really see providers dealing with in these reviews; improper coding is always a big issue, right? Upcoding, Unbundling, and Incorrect use of modifiers. We know about Modifier 25 and 59 are always big heavy hitters there.
CJ: Exactly!
Alicia: And then you know basically, you know, keeping up in the industry, we have a lot of providers and different specialties, right? So, we're seeing labs are getting hit really hard for like urine drug testing. And DME providers are always, you know, dealing with a lot of issues. So, really it depends on like the trends that are going on in the industry.
Another really big area, medical necessity is always an issue. It's like so critical for providers and practices to keep up with their local and national coverage determinations, what's required for the services that they're providing? Another one, big area, Inadequate or Insufficient documentation like we are always in our education, driving home the message like; "Look, you know, your documentation through, complete, accurate is critical," most of the time it's providers only line of defense Under audit, right?
CJ: Exactly!
Alicia: Yeah! I mean, those definitely are like the top, top areas. When we talk about inadequate or insufficient documentation, some areas that fall under that are missing signatures or inadequate signatures, time missing for time-based codes, that's always a big critical area. So yeah, I mean those are those are pretty frequent things that we see over and over and over in the reviews.
CJ: Yeah, and I've seen a lot of that too, especially like the urine drug screens. I have people reaching out to me about medical necessity for those. And the other thing you mentioned, the TPE audits, I find it interesting and you can kind of correct me if I'm wrong, but I've seen you know the MACs will list what their TPE audits have been. You know, they're usually doing this on a statewide or regional basis, right? Where they're looking at an issue, but they're looking at it usually in a lot of different providers, and they'll often publish kind of the results. They'll say; "We had an 80% error rate when we did all these audits and then sometimes, they're publishing, these are the main reasons why somebody didn't pass the audit," and it's things like you just said, right? Lack of documentation. Sometimes practices don't even send in any documentation or it might be medical necessity and those sorts of things. Do you find, is that accurate what I just said? and do you find that really helpful to be kind of looking at the MACs and seeing what they're looking at?
Alicia: Yeah, I mean absolutely! And the MACs even publish what they're looking at, right?
CJ: Exactly!
Alicia: So, you can go to their website, you can pull up their TPE audit. Just exactly as you said and they list there, you know, even of late, some of the MACs are looking at evaluation and management services, like that's applicable to all providers, right? I think one of the big misconceptions about the TPE audits is that they are educational activity only, but providers really need to realize that there can be very significant repercussions for continuously failing those TPE rounds, right?
I just spoke at Healthcon for AAPC, we did a deep dive. There was this was a very hot topic. There were a lot of people came to that session that are dealing with these types of reviews. I think anytime you are subject to a TPE audit, they should be taken very seriously. I think it's also important, CJ, that folks know like; "Look, if you don't respond to an audit, that's an automatic failure." So, one of the one of the women who participated in that session at AAPC said; "They actually ended up setting up a PO Box, so that they could receive all requests for documentation to like streamline their process because they found in their organization the mail was coming in, but those requests for documents for not getting to the right folks, right?" So, I think that's a great take away for today as well, like making sure the right people are getting the request for records understand like you have to comply if the payer contractually and specifically with Medicare if they're asking you for records, then you're obligated to send them the documentation. You know, that's a critical component.
CJ: Yeah, that's exactly right. Like I often get calls from clients they want me to help them out. Like it's like, you know, they're already way down the line where they failed to respond to the 1st letter. They failed respond to the second letter. Now it's 100% error rate. And now they're being asked to return thousands and thousands of dollars. And now all of a sudden, they take notice. And so, it's like; "Uhm, you guys, you didn't even get your team on the field when the game started. The game starts, whistle blows and the clock is ticking when you get that first letter."
Alicia: Right!
CJ: And so, to your point, I've seen that over and over and over again and with the mail coming to you know, the address that's on, you know this is Medicare issue, right? It's whatever the address is when you applied for Medicare, right, to be a provider or your practice or your MPI and so it's like you got to make sure that the people who are getting the mail get it to the right people just so you can get in the game.
Alicia: Absolutely!
CJ: Otherwise, you missed the game altogether.
Alicia: And you see, even like in the Medicare appeal process, right? There are 5 levels. We talked about the different types of audits, right? Like the target probe and educate, the UPICs are way more I think, not that TPEs isn't serious, because a lot of times those types of audits escalate providers up to UPIC reviews. Medicare is not messing around anymore, right? They really want to get out of the pay and chase game, as we say. So, you know, failed TPE audits can land providers on prepayment review very resource and labor intensive for the practices. But UPIC audits have the ability to extrapolate. So, like you're saying, right? Maybe the audit it's statistically valid. Maybe, you know, whatever your error percentage of error rate is, now you know Medicare is going to extrapolate that back across your patient population and actual overpayment of a couple 100,000 can turn into a million very quickly. So, those are really critical to make sure that you're staying on top of those. Even in the appeal process, right, the five levels of appeal, just like you say, you have a window of when you can respond, and if you don't respond within that window, you may lose your appeal rights. So again, another critical component to get into the game quickly.
CJ: Yeah, and you mentioned around the TPE audits like it could be as general as E&M, right? That applies to all specialties or they can be very, very specific. So, I was working with a client in the northeast of the country that their TPE had to do with a drug and it's a very expensive drug that and they were treating rheumatoid arthritis, and so there's infusions that you give with some of these very expensive drugs. And what I found super interesting is that the MAC, it felt like the MAC couldn't find anything wrong in the records. So, this is what they did, they went to the drug insert. So, you know, whenever you get a drug, you know that and even if you get over the counter drugs, we all know those medication inserts in that very, very fine white paper and it's super, super fine print about all the contraindications, all the risks, you know, 2% of people experienced this yada yada yada. Well in that for this particular drug, it's recommended that patients get a TB test before you begin the infusions because that particular drug could make somebody immunocompromised. Well, Medicare was denying the drug because that product insert said you should be doing a TB test and they weren't finding a TB test anywhere in the records.
Alicia: Oh, wow!
CJ: So, I had never seen that before, so it point I wanted to make is like you can get very general types of things that apply. And if you look at a bunch of TPEs from MACs all over the country, sometimes it's like they're sharing information with one another, cause it seems like they're all looking at the same things. And then there's some very, very specific things.
Alicia: Well, you know that's one of the big issues or complaints about the TPE reviews is that each MAC has a wide expansion of liberties that they can pretty much make it up as they go, right? Exactly like you're saying. And to TPE, again, right? Basically they focus on one area or issue or service and providers can be subject to multiple TPEs at one time.
CJ: That's right.
Alicia: And the lab, I would say in the lab space, you know, I have some clients, I think another big area that providers really need to be aware of is that Medicare is invoking their tool, but opening their toolbox and invoking their right for provider enrollment revocations and preclusions, right? So, we've seen I have a client who went through the audit process. They went through, not very well, went through a UPIC audit and you know, after three failed UPIC audits. It's like 3 strikes and you're out of here.
CJ: Yes!
Alicia: Medicare, we are seeing more and more providers getting revocation and preclusion letters and those are a bear to deal with.
CJ: Absolutely! And you're probably going to an interested in if you would recommend this as well, but I recommend to people that if you feel like you can't handle the audit and provide what ammunition is needed to kind of fight against the audit, get somebody in there right away, like get a consultant like you or get somebody in there earlier rather than later, because when you're earlier in the process you, you might be able to have better results.
Alicia: Oh, absolutely! You know, we talk about like the appeal levels of appeal. One is going to be, you know, you can ask for redetermination, you can ask for reconsideration. And underaudit I mean, I can't stress enough how important it is to get an experienced healthcare attorney, right? Don't call your real estate attorney to help you with the Medicare office. That's you know, I always say like you can't go to a, you know, hip surgeon if you need a hand surgery, right? So, find someone who knows that who's very fluent in the game.
CJ: That's right!
Alicia: Get some experts in there. Get the expertise in there to help you, because especially in those extrapolations, right, like sometimes, yeah, maybe you're not going to be able to overturn the whole thing, but if you can do some damage control, poke some holes in the extrapolation, go after the extrapolation process, like very, very critical to bring in the experts, you know, when you're dealing, you know, depending on the complexity. I think really drives that as well.
CJ: Exactly! Look, let's take a quick break and then I want to come back and talk about those 5 levels of Medicare appeals. So, bear with us, everyone for a quick break and we'll be right back!
Welcome back everyone from the break we have been talking about these Medicare audits and at least I wanted to, I know because you get involved kind of at a very granular level with clients, can we talk about those 5 levels of Medicare appeals you kind of already alluded to a few of them, but maybe we can dive a little bit deeper if you can maybe just tell us what those levels are first and then maybe we go back and start with level one and then dig in deeper to each one of these.
Alicia: Yeah, course, absolutely! You know, again. So, five level levels of Medicare appeals and honestly, because some of these levels like at the ALJ level, the higher levels of appeal were so backed up, is really why Medicare came out with the TPE audit program in the 1st place, right? To try to mitigate some of those denials and some of those appeals.
So, the five levels, the first level is a redetermination, right? Providers once they receive their audit, the findings they have 120 days to ask for an initial redetermination. Which means, you know, they're going to send it back to the to a different reviewer within the MAC, and then they're going to review that, and then they're going to come back to you with their findings. And if a provider is still dissatisfied with the redetermination or the decision, you can ask for the second level of appeal, which is a reconsideration, right? And you have 180 days after you receive the redetermination decision to file for a reconsideration. This is a very important level, right? This is where you are going to have the opportunity to submit additional information. This is where you can bring in your consultant and your auditors, you know, your auditors’ results. When you get to this level, you definitely want to have health law, law attorney and consultants helping you here.
If you go through the reconsideration process and you're still not happy, and the reconsideration process really that gets sent out to what we call a quick, right, a qualified independent contractor which is completely separate entity from the map, right, they do like an independent review.
The third level is an ALJ hearing or administrative law judge hearing. Again, if you're not happy with the reconsideration decision or it's unfavorable, you can ask for an ALJ hearing. Providers have to request that hearing within 60 days of receiving the reconsideration decision. Again, that's why it's critical you have to stay on top of all of this, right? I can say in our experience the ALJ hearings are pretty backed up, right? There have been delays in the appeal process, significant delays in the appeal process. I remember a few years back that there were even, you know, they were taking some steps to try to mitigate the amount of these and getting some quick decisions out on them.
Again, so the fourth level is the Medicare Appeal Council review. Again, if the decision is not satisfactory to the provider, they can request a review by a Medicare Appeals Council. You have 60 days to request that, for filing for that.
And then the fifth level is a judicial review, right? If you go through the process of the 1st four levels and you're still dissatisfied with the Medicare Appeal Council decision providers can ask for a judicial review. That's a final, you know, your case goes before a federal judge for a final determination.
So, again the five levels are redetermination, level 1, reconsideration is a level 2, ALJ hearing or administrative law Judge hearing is Level 3, Medicare Appeal Council review is level 4 and then the final and 5th level is a judicial review.
CJ: Yeah! Thank you for that summary and hopefully everyone that's listening can understand how complex this is, especially if this is kind of the first-time practice or somebody's going through this. This this is really, really helpful Alicia to kind of get a high-level view of this and to take your advice of getting the right people involved early because you might think it's just a small little thing, but they can extrapolate, right? And they can make it into a bigger thing and they're not just doing this because they want to help you.
Alicia: Right!
CJ: Like there may be some of that in the education portion of a TPE, but they're after this stuff like there's a reason, they're looking at it and you know, it could turn out that you do just fine. I'm not trying to scare people, but I've just have gotten involved with so many of these that it's like they're serious and they're like, they're trying to change your behavior, essentially.
Alicia: And I think too, you know, like I'm kind of get teased a lot by my colleagues that I've kind of like I'm famous for this quote, but one of the biggest things that I always say is like; "Look, just because you got paid doesn't mean you should have, right?"
CJ: Exactly!
Alicia: If that was the case, we wouldn't have the need for all these post payment reviews. And, you know, improper payments and all this like, I can't stress enough and we're always on our soapboxes and we're shouting out, you know, get a compliance program in place, like, look at all of these things and you're practice proactively because honestly, you know, if you get to this point, you know our honest feedback to providers when we come in like; "Look, we're going to do an independent initial assessment, but you know, we don't have a Magic 8 ball. We can't wave a wand and make things all better for you. Like, we can only work with what you give us."
So, getting out in front of this, proactively getting your documentation, understanding the services that you're rendering and what's required. Like if Medicare is not like a big guessing game, if they say something has to be there or done then it should be there. So, give us something to work with so we can help you.
CJ: That's right, absolutely. Exactly! So, let's say we finished all the appeals process, whether it turned out well for us or not, let's say all of that's now in the past, you mentioned a compliance program. Tell us a little bit about what you would recommend people do to kind of prepare or prevent these things from happening in the future.
Alicia: Yeah, right? Like now more than ever, compliance programs are so critical. I mean, we've been seeing how they're required to have a compliance program. You know, you can't just have your book on a shelf full of dust we always say that, it really, there's the OIG, even the states are coming out like; "Look, your programs have to be implemented!" What does that mean, right?
CJ: Right, right.
Alicia: Practically, policies and procedures, education and training, and then the most critical component of, I feel, in my opinion, of a compliance program is you're auditing and monitoring, right? You need to be doing that internally to make sure that all the other controls that you're putting in place are effective and working. You know, understanding like what levels of service are you providing? What types of providers do you have? What's going on out there in the industry? What are they looking for proactively, looking at your coding and your billing, and making sure that you're in compliance, it's critical.
CJ: Yeah, you know, and one of the things I tell clients is; "You know your business better than anyone. So, get with whoever you know understands your revenue intake." Is it E&M that predominates? Is it a certain procedure? Let's say you're a pain management doc and you do a lot of spine injections. OK, if that's kind of one of your major services. So, what I tell people is; "Find your major services and then look for any LCD or NCD that covers what you do. Then read those things like you are studying them for an exam because you want to read the narratives," like you just said.
Alicia: Exactly!
CJ: It's if you get paid, that doesn't mean things are hunky dory. That might mean, you're getting paid, Medicare assumes you're meeting all the requirements of that LCD and it's not until the post payment review that you get in trouble. And I bring this up as an example because like for pain management and those spine injections, most LCDs will say something in there of, you know, before you can do these injections. And before Medicare considers the injections medically necessary, you have to demonstrate three months of failed conservative treatment and failed therapy options. Well, that's in the narrative of the LCD. So, you're not going to get that by kind of matching up codes. You have to see; "Oh, wow, they expect all of this to be in the medical record even before I do this service." And so that's what I kind of reading those LCDs and NCDs and you alluded to it as well. That's what I would do if I were in a practice, I would see what are my main major services and do any of those have LCDs or NCDs? That's at least where I would start. What do you think about that?
Alicia: Absolutely, yeah. Critical, right? I mean, those are the coverage determinations. Those are the guidelines. You know, I have to say I was asked to do a webinar for decision health on the Medicare expansion codes that came out right, like some of the social determinant of health assessments and the PIMMs and some other, you know, new services that are available to providers. And you know, I was like sure, you know absolutely no problem. And where do you go to get the information on that right you go to the Federal Register, you go to the physician fee schedule. And just like you're saying the LCDs, the NCDs you have to get in, really get in there and understand what's required of you before you just willy nilly start rolling out and billing for services. There are in those types of services I was like; "Wow, this is really in depth because yeah, you can do these services or component of them incident too, which is another big area where providers fall off the cliff, right?
CJ: Yes!
Alicia: Understanding like, what does that mean? You know, supervision and incident two are very different things, so get to the source, go right in there. Like you're saying, like bedtime reading but there's no substitute for educating yourself in advance and being prepared before you really put yourself at risk. And I, you know, I never forget, like the HCCA conferences I love, you know, and I always loved going and listening to the Inspector General, right? You're getting information right from the horse's mouth and, you know, one time, he said in the beginning of his speech it's like; "Look, if you're not really sure what your risk areas are. Like, follow the money because that will always be your biggest risk area in any organization." So yeah, the revenue cycle is the is the artery of your practice and you know getting that crush could really do some significant damage.
CJ: Exactly! That's exactly right, yeah! I spent my career in compliance, but I was real close friends to all the revenue cycle folks because I would ask them, you know, let's do the 80-20 rule, what represents 80% of our revenue. And usually you could get, you know, a list of 8, 9, 10, 11 types of service lines that represent that 80%, you know, put your money, your resources, your auditing and monitoring time in those areas at least start there and to events that you're that you're doing it right.
Alicia Yeah! Absolutely! Anybody who tries to say about the revenue cycle is not a critical component of a compliance program, is very mistaken, right? It's one of the biggest risk areas that your program really has to include that.
CJ: Absolutely! Alicia, we're getting a little bit towards the end of our time here, but I want to see if there's anything else that you think might be really important. You know, you talked about kind of, you know, letters, consulting with experts, what from all of the things that we've talked about. Any kind of key takeaways or other thoughts that maybe I didn't ask you about?
Alicia: No, you know, I think really like just with the whole you know audit and appeal process compliance overall in general like when it comes to the audit piece of this, I want to say you know critical like some key takeaways understand the audit findings, right? Dig into those understand what's happening. Get some experienced folks on board folks on board to help consultants, experience health law attorney, take him seriously, right? Designate someone to oversee and manage these reviews. Gather all the documentation. Get into those policies proactively. Hopefully, as we were talking about, you know, preparing detailed letters, make sure you're meeting your deadlines, right? Be mindful that there's timelines like you said, I mean, I actually got a call from the client last week for help with an audit and I'm like; "Okay, well, when do we have to respond?" Well, "Oh! In seven days." Like, "What are we going to do in seven days, right? So, we're going to have to ask for an extension. Okay, hopefully the auditor's going to be nice and they'll give us an extension."
CJ: Exactly!
Alicia: Get out in front of it early, right? And then learn from everything that's going on, learn from the audit, especially TPEs. Take advantage of the educational components to those participate in that. And you know, I don't know, my big my biggest take away I could say for everyone is just get out in front of all this proactively, you know, be prepared, be audit proof right, be audit proof. That's what I want to say.
CJ: Yeah, exactly! And, you know, learning from your own audits, but then also you referenced this as well, learn from other audits that are out there that are might be in your same lane, so you know you might be reading, I do this all the time I'm kind of a nerd, I read all of the press releases of what the recent settlements are. I'm trying to read audit results from OIG. You know, you're in New York, OMIG, New York office of Medicaid Inspector General. They have audits that they do on their website.
Alicia: Definitely!
CJ: So, it's like, look at what they're investigating. And then if you fall into that space too, do your own investigation internally before they come to you.
Alicia: Definitely! Oh, right, yeah! I mean, it's one of the best ways to figure out what's going on out there, right? I mean, yeah, what are they looking at? It kills me every single time. Like, I see a laboratory who's getting hit really hard with like these definitive drug testing like codes that they're building like that's been out there forever.
CJ: Yes!
Alicia: Like, how can laboratories not be like read the, like, reading the news and someone in the organization should be staying up on all of this to mitigate your own risk? Absolutely!
CJ: Exactly. Yeah, spot on. Well, Alicia, you have been just a treasure of knowledge and information and experience because you've mentioned you've been doing this for decades. Thank you so much for being willing to share your thoughts and opinions.
Alicia: Oh, super fun. Thanks for having me! I really appreciate it, CJ.
CJ: Yeah, and thank you to all of our listeners for listening to another episode in our parting message, we always say this, you know, if you have topics that you would like to hear more about, please let us know if there are speakers that you think would be great guests. We're always looking for that and we'd love to hear your thoughts and so thanks everybody again, until next time, please take care.