Episode 99:
Expert Insights on E/M Coding
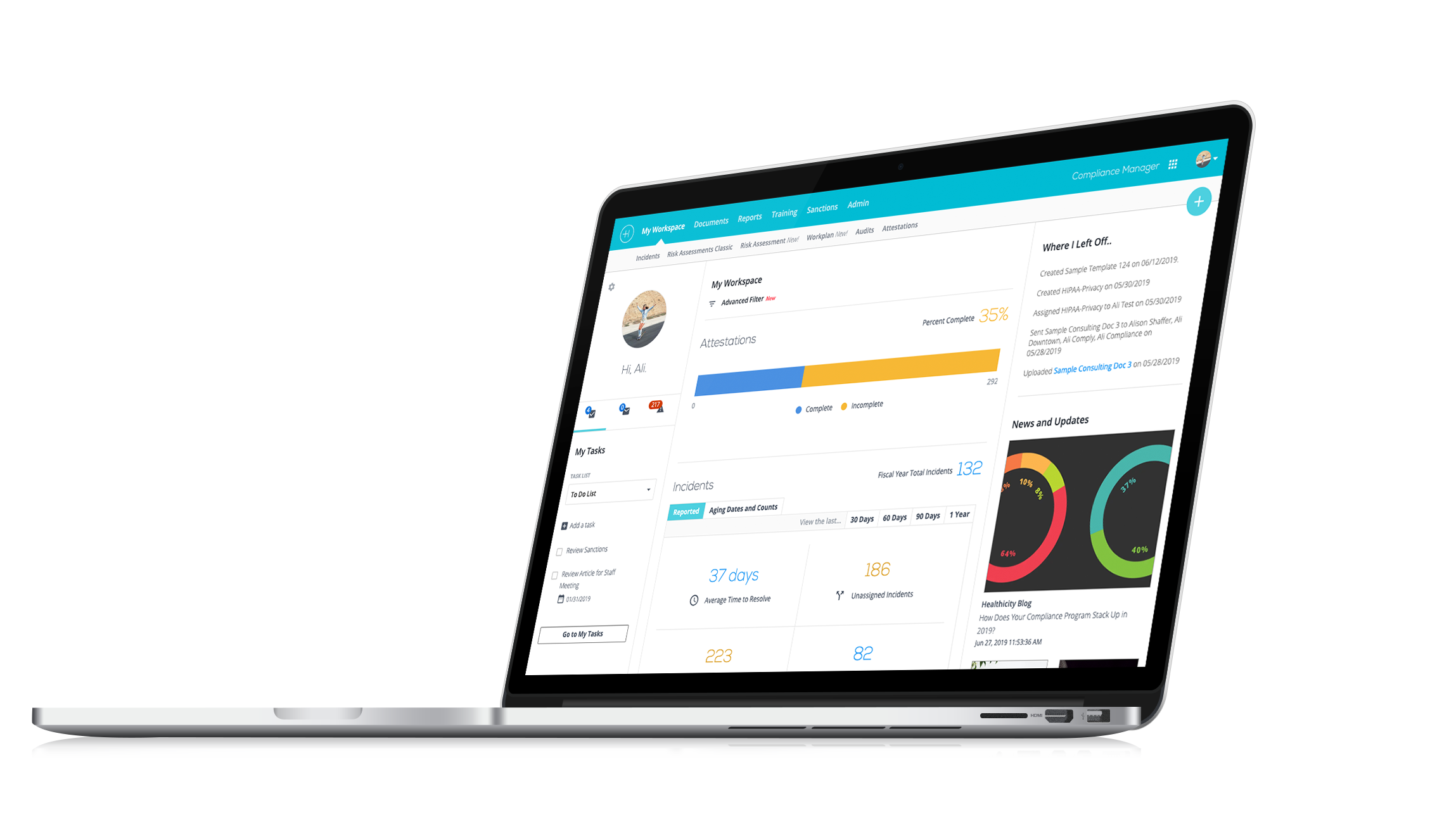
Watch the demo:
Compliance Manager
See the only all-in-one compliance solution today.
Tune in for insider tips and strategies for mastering Medical Decision Making and tackling documentation challenges with E/M coding!
In this episode, CJ Wolf, MD, and E/M coding expert Sharisa Freeman discuss her journey and insights into mastering the complexities of E/M coding.
Here's a quick look at what you can expect from this episode:
- The Evolution of E/M Coding: Changes in guidelines that shifted the focus to Medical Decision Making.
- Medical Decision Making Tips: Understanding the three essential sub-elements: number of problems, data reviewed, and risk.
- Documentation Challenges: Common issues with lower-level visit documentation and how to address them.
- Networking and Continuous Learning: The value of staying updated on coding changes and connecting with peers.
- Advice for New Coders: Sharisa’s top tips for those just starting in the field.
Check out their conversation today – and thank you to Sharisa for sharing her time and insights on Compliance Conversations!
Interested in being a guest on the show? Email CJ directly here.
Episode Transcript
CJ: Welcome everybody to another episode of Compliance Conversations. My name is CJ Wolf with Healthicity and today's guest is Sharisa Freeman. Welcome, Sharisa! We're so glad you're here!
Sharisa: Thank you! Thanks for having me!
CJ: Yeah, absolutely! I really appreciate your time and you're all going to learn a little bit about Sharisa and her expertise. And I think it's going to be a really interesting topic. So, Sharisa, one thing that we like to do on the podcast before we kind of jump into our topic is we just want to get to know you for a second, so if there's anything you want to tell us a little bit about yourself, like we all kind of come to this space from different paths, right? Like, who grew up thinking; "Oh! I'm going to end up in this space 20 years from now!" I didn't even know what it did, right? So, anything you want to share about where you come from, your professional background, anything like that that you want to share.
Sharisa: Yeah, sure! Hi everyone! Where to start? Yeah, I actually did not expect to be a medical coder, so that was something that kind of took me in another direction. Well, I've been coding since 2016 full-time. I started in 2014 as a temp, and got hired on full-time with where I'm at now, so before that I had pretty varied background. I had extensive sales, customer service and actually was postal worker for a bit.
So that was kind of a challenge. And at the time my son was young, very young before starting school, and I wanted to be at home with him. I worked 13 hours a day, 7 days a week pretty hard for a new mom, so I wanted a job where I could, you know, make a substantial salary and still be a mom. And this came up and it started out as a, you know, I went for a temp job for administration and they were like; it's at a hospital. I have no hospital experience. Yeah, yeah, yeah. I'll just go, you know, you, you just want a job.
CJ: Exactly!
Sharisa: I went and for two years, I walked around the hospital campus signing people up for the patient portal and talking with patients and getting feedback to take back to the heads of the hospital every week and they were like; "Hey, you should be a coder!" and I'm like; "No, I shouldn't. I don't know about that." But they offered to pay for everything, the class, the materials, and so I went.
CJ: That's great.
Sharisa: Few months, few months later, sat for the test. I passed on my second attempt. I missed the first attempt by like 1%. And the boss was like; "Wow, that's pretty great. We know doctors that don't pass!" So, and they offered me a job and I started learning general Pediatrics coding which they thought was easy. But peds is not really easy.
CJ: I know, right?
Sharisa: Yeah, fast forward today, I do general internal medicine coding, professional billing and I help with denials. And do some hospital denials as well.
CJ: Yeah, and Sharisa and I met because she's involved in her local chapter. And I think that's great service too, that you're doing. So, we really appreciate the work you do there to help others. And that's a great part of this profession, I think, too. It's fun too.
Sharisa: Yes, it is. I think it is and it's really helped me to grow in my experience as well as on-the-job learning. But it's been really great to network with a lot of professionals and really get the ends and nuances of it.
CJ: Exactly! Well, thank you for sharing a little bit about yourself. So, most of you can probably tell that she's got lots of experience. So, we're going to talk a little bit about today about E/M coding, right? This is a big topic. We've all dealt with it. If you've been in professional coding or billing for a long time, it's like this big topic, right? And I know you have a lot of experience there.
Sharisa: Yeah, I think for a while they were talking about getting rid of E/M coding and I don't know if you remember those articles and talks about that, and turns out it's not really so easy to cut that out because it's kind of a lifeline of way of coding. I think you know; everyone goes to see their primary.
CJ: Yeah!
Sharisa: And you know, so specialist, it's just it's the basis. So, it's like you can't get rid of the foundation, I think.
CJ: Exactly! Because there's so many, you know, providers who don't do a lot of procedures right, like so if you're a surgeon, okay, I could see that getting rid of it might work at some form or fashion, but so many doctors and providers are, you know, the bulk of what they do is they take history, they do physical exam, they think through problems, they figure things out. And there's complexity there. And so that's really cool. So, if somebody didn't know much about E/M coding and you had to like just in a few sentences or words any high-level thoughts before we dive deep, what would you?
Sharisa: Oh! I don't know! I usually try to. E/M is usually when you say E/M, everyone's like; "Oh, God!" And it's really daunting and I get it because for the first, oh my goodness, the first several years like 3-4 years, I would every day, I'm like, I don't know what I'm doing! Like, you just have that feeling like you don't really know. And it took for me.
CJ: I know. Exactly!
Sharisa: What my trainer did is I don't know if you remember the audit tools, the 95-audit tool I have to print those and I printed them and for each patient that I worked, I had to manually like fill out one of the audits tools, and I think that that was a really good way to understand the elements, the risk and diagnoses, just the different components that make up E/M coding and that helped me a lot. So that way it got to where I kind of knew the sections by heart and certain things just kind of fall into place because it is sort of repetitive what we do, after all, it's a bit repetitive at the base and that helped me a lot where, you know, it's just a matter of understanding how to equate the checkboxes to your information on the patient chart because doctors as you all know, everyone documents differently, their wordings different and just knowing that and knowing that as a coder, you're not allowed to assume anything, you take it for face value.
CJ: Right!
Sharisa: And I think if you can do those things, E/M it's not so bad, and then you know now here I am, I'm okay. And what it did really help when they got rid of the audit tools. So, I know that was a big chunk of it. But usually when I tell people with E/M it's, you know, because my friends would ask me; what is that? And I'm like, you know, you go to the doctor and; Oh, I'm here for a check-up. But I have this cough and my arm is hurting or I've been feeling dizzy lately. And I say; you know how they're sitting there just typing, they're typing everything you're telling them, then they examine you and then they take a look back at your history, if you've been there before, or if you're new, they look at your, you know, you get everything requested or whatever, and they just make an assessment. And then what I do is I take all that information, and convert it into alphanumeric codes to send off to the insurance payer.
CJ: I think I've had that conversation, that exact same conversation like my kids will be like; now what do you do, Dad? Like, really? What you do? And I was like, yeah, I and what you just described is exactly what I tell people and I think that's a perfect, a perfect description. You kind of mentioned your experience before these, you know, we all know the E/M guidelines, maybe not everyone listening knows that the evaluation and management guidelines for years, and you referred to this used these 1995 or 1997 guidelines which were different documentation guidelines in 2021 and in 2023, that changed a little bit. So, I maybe wanted just to ask you because it sounds like your career has been long enough, you did both.
Sharisa: Yes.
CJ: Are you happy that change went through? Are you sad? What do you miss?
Sharisa: I'm very happy, I'm very happy in the sense that, it's just I think it's simpler because it was so much stress on providers to have all of these notes chalked full of information and a lot of it might not have been as relevant to that day's visit and having to weed through all of that is it's a lot. And then with them having to document so much, it's taking away from actually examining and just really taking time to really make a better assessment for that day. And I just think it's better and I know that was one of the benefits we talked about that in our chapter when we were presenting the turnover, the changes, and how, it's a benefit you know, yes, we still want you to document everything but now the focus can be on medical necessity versus just trying to fill up a page, you know what I mean?
CJ: Exactly! Yeah, see, I started back in 1999, and I feel the same way you do it. It seems like, you know, doctors were like; Oh, did I get enough review of systems or did I do HPI elements and they were so focused on that, that it's like; know the real reason you do what you do is to make your medical decisions. So, do what you feel is the right history, do what you feel is the right exam, and then let's focus on your medical decision making and you know, you and I have been in, you know I was presenting a class I think for your chapter where we were talking about kind of working through that medical decision-making process. I think that's a little bit more natural doctors, like I think, you know, it probably was hard for some docs who had been doing it one way for years, and now they're told to do it a different way, but if you're a brand new doctor just starting to learn about this, I think it makes more sense to think about these things as a medical decision making type of exercise as opposed to did I hit the boxes and review as systems.
Sharisa: Yeah, you bring up a good point. We have a lot of our physicians who are, you know, one physician that I coded with, he has retired now, he had been doing it for so long. So, he was so used to a certain way and sending all of these queries and in-basket messages every time for each of his notes. And he would just get so annoyed. And so, we had to have all these meetings and what we would do, we're split up into teams. And so, the team that I'm on, we would meet with our, I guess for lack of a better term, we meet with our liaison or our coordinator, the person that talks to the clinic directors for our group.
CJ: Right!
Sharisa: Because you know and like our, I think we're, I'm under the internal medicine group. So, we have a clinic director, and then that person would relay these changes to all the physicians and kind of go back and forth with us. So that was quite an adventure and it took a while. But I think that as you mentioned now they see that it's just flowing much more easier because yes, we still want you to document. Yes, don't leave anything out if it's important to the visit. But you don't have to put all of you know, so that's it's so much better now. I love it!
CJ: Exactly! I do too. We're going to take a quick break and then we're going to come back and maybe we can dig a little bit deeper into medical decision-making if that is good for you. So, hang tight everybody, we'll be right back!
Welcome back from the break, everybody. We are talking to Sharisa Freeman, who's an expert in E/M coding, and we were talking about E/M coding in general and we talked about how we kind of both like that medical decision-making is a little bit more of the focus.
When you think through those three sub-elements, right? Number of problems and complexity, data reviewed, and risk. Is there anything that pops out to you in those three, do doctors and coders struggle more with one or the other? What are your thoughts just in general about those 3 sub-elements?
Sharisa: Well, that's a good question. I have quite a few. So, I think I'll start with the providers I work with in my clinic, a lot of them struggle with the lower level visit, so if it's a low or straightforward, they struggle with that and the documentation supports a higher level because again with the new model, for anyone who doesn't know, if you meet two out of the three elements, it's automatically that level, so if you have an element from a moderate data and moderate risk, you're going to code that as a level 4 visit. So, that could mean; Hey, I looked at three different labs or I ordered 2 labs and then I looked at another one. Because they're coming in for chronic diabetes, so the patient has diabetes, it's not progressing or anything. It's just kind of going along its route. But of course, with diabetes, you have to come in more often. You're going to look at more tests.
CJ: Right!
Sharisa: Put those three tests, and the two tests you look at, the one you order. That's all relevant to why they're there. So, you can't take that out to make it a lower visit and that so yeah, you can. It's just playing around with knowing what it is. And for me, I sent a lot of messages to providers where we can't build them. I work for a teaching hospital and the resident will see the patient, but it is a higher-level visit based on the MDM chart and because they weren't seen by an attending or billing provider, I can't send that. So, I send a lot of those out, but then the providers are reaching back like; No, no, I didn't need to see them. And so there's that. Then there's a case that, I actually had this morning, the provider tells me, you know, even though I'm mentioning these are the reasons that this should be a level 4, he sends me a message back; "Don't change it. It's a Level 3. The visit was really short." But your documentation says that they have multiple chronic issues, that are multiple stable chronic issues, and you adjusted their medication so it doesn't matter if you saw them for 10 minutes, 15 minutes, you did that within that short amount of time. And so, it's a moderate visit. So, that was something that happened this morning.
CJ: Nice! That's right!
Sharisa: And so, what we do is, I just mentioned I said well, current documentation does support a higher level. If you disagree, please adjust or update your documentation to reflect the lower level so that is a big area that I'm seeing.
CJ: Interesting!
Sharisa: Yeah, so it's funny like, it's so much easier for me and it could be because I've been doing this a while also, but you know, hey, two stable chronic conditions, you're coming in for a follow up on your chronic conditions. Oh, you told them to continue taking their medications, that qualifies as a moderate-level visit. And a lot of our providers may not like that!
CJ: Yeah, right! And you're now in primary care where that's so common, right? Like where they're having, like, you're probably, you could tell me, but you're probably seeing patients with more than two chronic conditions, right? It's like...
Sharisa: Oh, all the time. All the time. Yeah, it's internal medicine, so yeah, off the bat, they've got the first three main things, diabetes, hypertension, chronic kidney disease. That's three. And just off the bat. So, yeah, usually...
CJ: Right!
Sharisa: Yeah, my diagnosis list can be like 12 items, 14 diagnoses typed in, and so it's quite a lot.
CJ: Yeah! And I was actually meeting with a physician group trying to teach a little bit about E/M coding recently. And we had this conversation and I said you guys are so fast in your mind to work through all this. So yes, it might be a quick visit, but you actually did all that work. You did it in your head. You evaluated those 3 chronic conditions. You did look at their medications. You did have to consider; yeah, they're improving or they're stable. So, I need to either keep them on this med dose or a different dose. And that's just so common in primary care that a lot of those are going to be for established, right? They're going to be level fours.
Sharisa: Right! And that's the area of issue and I'm not sure and maybe you'll have suggestions I could take back. But you know our auditors on our end just tell us to do as I mentioned, asking them to make their adjustments in their documentation if they want us to change it. Otherwise, it goes through at the level that it should be at. You know, it's because it's out of our hands. It's not that; okay, I'm so sorry. I'll change it. I can't do that. These are, you know, guidelines from AMA and you know, so.
CJ: Right!
Sharisa: That's kind of where we're at with that.
CJ: Yeah, you know, so I've also worked kind of in compliance departments too, where sometimes we have to make internal policy decisions or like operational decisions of who's the final person to decide, right? Like who has the final say and those sorts of things. And then making sure like you just said, having policies to say, look, these are the guidelines as an organization we're going to follow, this is going to be our policy. We're going to do this and it's going to be inappropriate. I wanted to ask you too, like on that data reviewed. So, I don't know if you've ever done like specialty E/M coding very often, but...
Sharisa: Oh yeah, I Oh my goodness. I've done oncology. I have so, peds, oncology, sickle cell, GI liver, and cardiology. Yeah, quite a few different areas. And I do help sometimes with inpatient coding too. So yeah, a little bit of everything.
CJ: Gotcha! Yeah, so like I was, this was an orthopedic group and they don't do a lot of labs. And so like, I'm thinking of that, that second sub-element, which is the amount of data reviewed, right? And for them that column or that element that rarely affected them, it was mostly, you know, that first column of the complexity of the problem presenting because they had this a lot like a they might have an osteoarthritis patient who's worsening. So, they're kind of meeting the moderate on that first element and then their data was rare like because they just weren't doing a lot of labs and tests, and so they rarely got much in that data. And then it really then it came down to that third column of risk. You know, whether they were just saying PT, physical therapy versus, you know, a prescription drug management. And so, we were kind of working through that. It does seem like though, I'm kind of curious what your thoughts are for the specialties that you just talked about. It seems like that data reviewed column probably does come into play more than like for a specialty though.
Sharisa: I think it does.
CJ: Yeah?
Sharisa: I've never worked in ortho, that's not what I'm familiar with. But I would say even with that, are they looking at any prior scans? X-rays that could be counted that could be counted if it's relevant, but that's the only one. I would see that they would be able to check the box for.
CJ: And we had that conversation that, like patients would frequently bring in an MRI or something from another doctor, and then they would personally review the image. And so, if you're personally reviewing that image and you're giving your interpretation and you're not billing for it separately, then you do get that kind of moderate in that column. That was the one discussion we had that was kind of the scenario when it kind of bumps them up in that middle column.
Sharisa: Yeah, because otherwise, that's a big one for ours because you know, they're running lab panels, obviously, they're looking at the blood levels, HbA1C, you know, and then test for liver enzyme levels just different things. So, they do get that, but the trick is in the beginning when they switched over to the new way of MDM coding, we were all getting tripped up over; I ordered the test and now I'm looking at it and so it was kind of like they were getting double marks for it, which was pushing it down to more of a higher level. And so, what our auditors did is they kind of did some research and they decided that; like in a typical note that I look at the provider will put you know all the elements HPI, chief complaint, whatever and then for the labs, he'll say; reviewed the following labs, but the labs were dated from like six months ago. So, we're supposed to look at; okay, you don't get points for ordering them if you didn't order them at this date of service. And then also you're reviewing these ones from six months ago, but are they relevant to why the person is there for that day? So then again, it's relevancy medical necessity was and so that's where we have to really kind of be careful, because I was pushing out so many level fours, because they're saying; "Hey, he documented that he reviewed all these tests," and the auditor is like; "No, but this is not, you know, the patient just came in because they have a rash or they're sneezing, allergies, whatever, but these tests are for their blood levels and some other things that were done before.
CJ: Right!
Sharisa: And so, it's not really relevant to the visit so that you know that was an area that we had to kind of really watch out for.
CJ: Yeah! Do you ever see very many scenarios where they reach that level 5 in primary care? And if so, what can you give any examples where that's happening?
Sharisa: I do. Mostly in oncology, there are some fives where we see level fives is time-based coding if the provider came in and they've spent time over what an hour or 90 minutes. And typically, I only see that in like somewhere oncology. Somewhere like that, or maybe cardiology depending. Otherwise, level fives that I'm seeing is if this person is coming in and they're being admitted.
CJ: Ah, yeah!
Sharisa: So, they're coming in with something that and even if you look at the level 5 elements, it's like this person needs immediate care and admission to the hospital. They have to be put on fluids, maybe they're hypotensive, you know, they're dehydrated. They are passing in and out of consciousness when they're there, it has to be something really high level that needs to be immediately treated, that is really going to directly affect their life. So, if we don't treat this, this person could, you know, expire or pass away. But then they it gets tricky with that because then you have to look at the insurance payers because government payers do not let you do a level 5 if they've been admitted that same day. So, what I've experienced is if the internal medicine coder saw the internal medicine provider saw them deemed it an emergency, admitted them and an internal medicine doctor admitted them through inpatient.
CJ: Gotcha!
Sharisa: The inpatient code for or the emergency code gets coded, and then we have to put in like a dummy code to show. If and, that's again for government payers like Medicare and Medicaid.
CJ: Yeah! That makes sense, right? Because if that office visit led to an inpatient admission on the same date of service, you correct me if I'm wrong, that kind of gets rolled into that initial hospital care code, right?
Sharisa: Yes! It does, same day. And I think, I don't have it in front of me, but like we went over in our meetings with our auditors. If they're admitted the same day and discharged, there's a certain way to do that, or if they're admitted into inpatient and they're staying ongoing
CJ: Yeah! Well, Sharisa, we're kind of getting towards the end of our time. I could talk to you all day about Your wealth of knowledge.
Sharisa: Yeah, there's a lot. Yeah, I'm just grateful that I know some stuff, finally.
CJ: Yeah! Well, you're an expert. Any last-minute thoughts or tips on E/N that maybe, I don't know if somebody's just starting in, in coding or I don't know anything that you have any thoughts that you might have?
Sharisa: The only thing I'd say is like I mentioned earlier, never assume anything. Always, never be afraid to ask questions. You know, encoding things change almost daily, so always keep yourself, you know, educated, updated on the changes in coding. AAPC has a lot of great articles and keeps us updated with that. Your local chapters are very good with that. And yeah, just always asking, just keep asking questions, and never assume anything, like it could, if it's not documented, it didn't happen. So, isn't that what we always say?
CJ: Yeah, right! That's great and that's great advice. And you know, you and I, you know, when we were doing your chapters presentation, you know, I think that was a theme too. Having coders learn as much as they can so they can help the doctors; "Hey, get that on paper. I can't assume it." But I think you're probably trying to say this. I'm not putting words in your mouth. But this is what I learned; "Is that true, and if so, can you put that in the documentation," and I think that like I've been doing this for so long, I think that's truly important to have those relationships where they're comfortable talking to you and you're comfortable talking to them.
Sharisa: Yeah, definitely, I agree. Because on the doctor's side, it's like you said, it's fast-paced, they're seeing these patients, they're going and they're documenting and we weren't there. So, we're seeing just everything after. So, yeah, I definitely agree with you on that.
CJ: Well, Sharisa, it's been such a pleasure talking to you about this. And thank you so much for your time and willingness to share.
Sharisa: Thank you! Thank you! You're welcome! And thank you so much. Oh, my goodness, I enjoyed your presentation you brought before as I mentioned, I had seen it on AAPC and I'm like; "Oh, my God, we have to share this with our chapter members." So, I was so grateful to you for coming out. And we look forward to you coming out again. I believe in November, I think it is, right?
CJ: Yep, yep. Love to do!
Sharisa: Yeah! We're looking forward to that.
CJ: That's awesome! Thank you for the invitation.
Sharisa: You're welcome!
CJ: And thank you all to our listeners for listening to another episode of the podcast. As usual, if you have topics that you think would be fun to have us discuss, please share those topics with us. If you know of guests like Sharisa that have expertise or experience in a certain area, please feel free to share their names with us and we'd love to maybe have other guests on as well. So, thanks, everybody! And until next time, please take care!