Compliance professionals often spend a lot of our time interpreting shades of grey. We may be asked if medical documentation truly supports “medical necessity.” Or whether there’s inappropriate intent accompanied with compensation of some kind as it relates to potential violations of the anti-kickback statute. Sometimes it can feel like the only answer compliance officers give is “it depends.”
However, there’s one area of healthcare compliance that is mostly black or white: Exclusion checks.
Did you perform exclusion checks on employees or entities who have worked for your organization? You should! It’s an easy win when it comes to compliance.
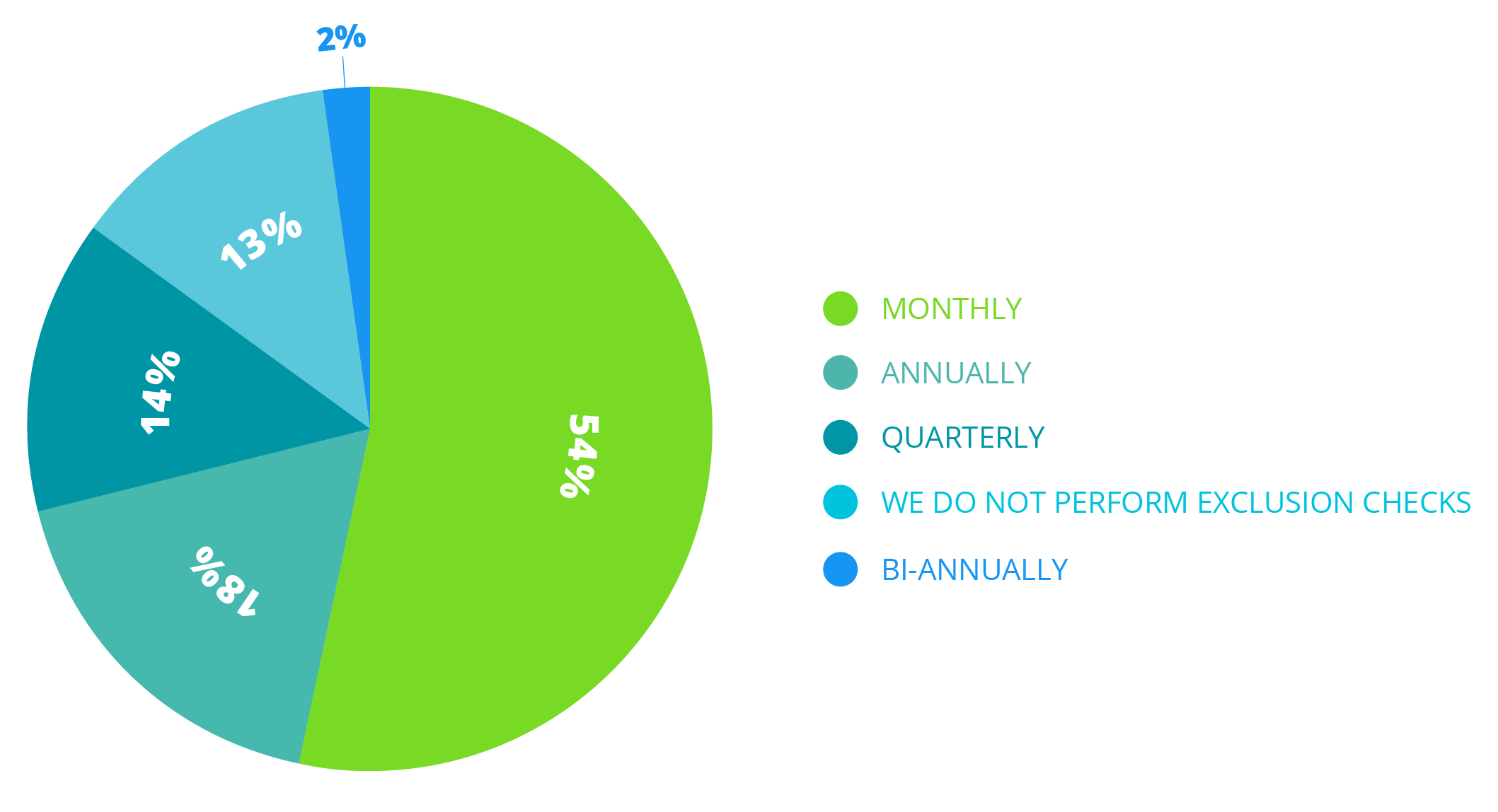
Surprisingly, Healthicity’s recent compliance survey found that 13% of those surveyed don’t perform exclusion checks at all. Shocking, right? If you’re like many of us, you probably read settlement stories regarding the OIG where an organization employed an excluded individual or entity. It’s never pretty.
For example, in April 2019, a Maine Mental Health Services company entered into a $17,750.12 settlement agreement with OIG that resolved allegations that they employed an individual who was excluded from participating in MaineCare, Maine's Medicaid program. OIG's investigation revealed that the excluded individual, a counselor, provided items or services to patients that were billed to MaineCare. It’s all downhill from there.
Download our free eBrief, Exclusion Monitoring: A Simple Compliance Win, to learn why exclusion checks are the simplest thing you can do to protect your organization from the OIG’s rath.



Questions or Comments?