Key Findings from the OIG’s Recent Hospital Billing Audit Report

For many years, the U.S. Department of Health and Human Services Office of Inspector General (OIG) has been performing hospital compliance reviews (https://oig.hhs.gov/newsroom/podcasts/hospital-compliance/). In practical terms, these are billing audits the OIG completes for select hospitals and specific types of services. Frequently, the OIG used data analytical methods to identify higher risk hospitals and billing issues originating from both inpatient and outpatient hospital Medicare claims.
In a recent audit report, the OIG created a summary of lessons learned from 12 of these hospital audits performed during 2016-2018. They wanted to determine the actions taken by the Centers for Medicare & Medicaid (CMS) regarding the OIG’s recommendations in these 12 audits. They also considered the results from the first and second level of appeals to determine whether identified claims errors were sustained. Lastly, OIG wanted to confirm that CMS is making the best use of their reports to increase its oversight of the Medicare program.
Did OIG audit findings stick after hospitals made their appeals?
In the 12 hospital compliance audits selected from 2016-2018, OIG identified 387 improperly paid claims. 333 of those were inpatient claims resulting in $5,260,147 in net overpayments, while 54 were outpatient claims resulting in $53,729 in net overpayments.
Of the 387 improperly paid claims identified by OIG, hospitals appealed 229 claims at the first level and 22 of those overpayment determinations were overturned. In addition, 126 claims were appealed at the second level and six overpayment determinations were overturned.
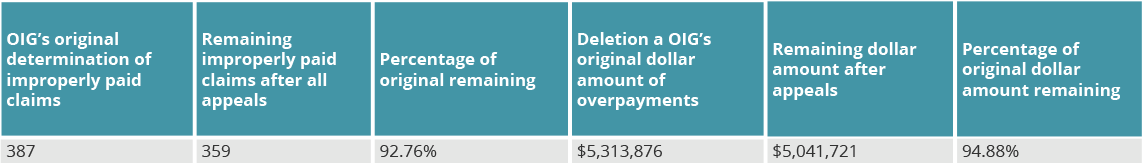
This resulted in 359 of the 387 remaining overpayment determinations. These remaining claims resulted in sustained overpayments of $5,041,721. Because the claims were a sampling from a larger universe, OIG determined that the total overpayments received by the 12 hospitals was $82 million.
After performing some simple calculations, it appears that after all appeals are accounted for, the remaining percentage of the OIG’s original findings were approximately 93% for the number of claims and 95% for the dollar amount overpaid (see chart).
What were the most common errors?
For the inpatient errors identified by the OIG in these past 12 audits, the most common errors were for Inpatient Rehabilitation Facility claims. The next most common inpatient error was failing to meet criteria to bill the service as an inpatient stay. In other words, the services should have been performed and billed as outpatient services. And the third most common error was reporting inappropriate Diagnosis Related Group codes. Specifically, the medical records did not support certain procedures or diagnosis codes, resulting in overpayment. The chart below includes a detailed summary of inpatient errors.
Hospital outpatient claims also demonstrated frequent errors. The most common error type for hospital outpatient claims was reporting incorrect HCPCS/CPT codes. The second most common error was incorrect usage of bypass modifier, such as modifiers 59, XE, XS, XU, and XP.
What is the OIG’s 60-day repayment rule?
In most audits performed by the OIG resulting in overpayment findings, the OIG recommends the organization exercise reasonable diligence to identify and repay overpayments during a six-year lookback period based upon credible information of potential overpayments.
A typical OIG 60-day rule audit recommendation states that the provider, “based on the results of this audit, exercise reasonable diligence to identify, report, and return any overpayments in accordance with the 60-day rule and identify any of those returned overpayments as having been made in accordance with this recommendation.” In other words, the OIG is emphasizing the 60-day rule that requires providers to look back six years to determine if identified overpayments span that six-year lookback period.
If you have not reviewed the 60-day rule recently, you can view it here: https://www.federalregister.gov/documents/2016/02/12/2016-02789/medicare-program-reporting-and-returning-of-overpayments
Conclusion:
There are a lot of lessons hospitals can learn from this most recent OIG audit. Any hospital compliance professional can benefit from reviewing this report and identifying potential improvements for their own program.
Download this blog as a PDF, click the button below.


Questions or Comments?