Deeper Than the Headlines: Hyperbaric Oxygen Therapy
compliance, OIG, medicare, RAC, Recovery Audit Contractor, CMS, deeper than the headlines, documentation, MAC, LCDs, Medicare Part B, HCPCS, OIG Report, Medicare Part A, oxygen, Hyperbaric Oxygen Therapy, Oxygen Therapy, HBO
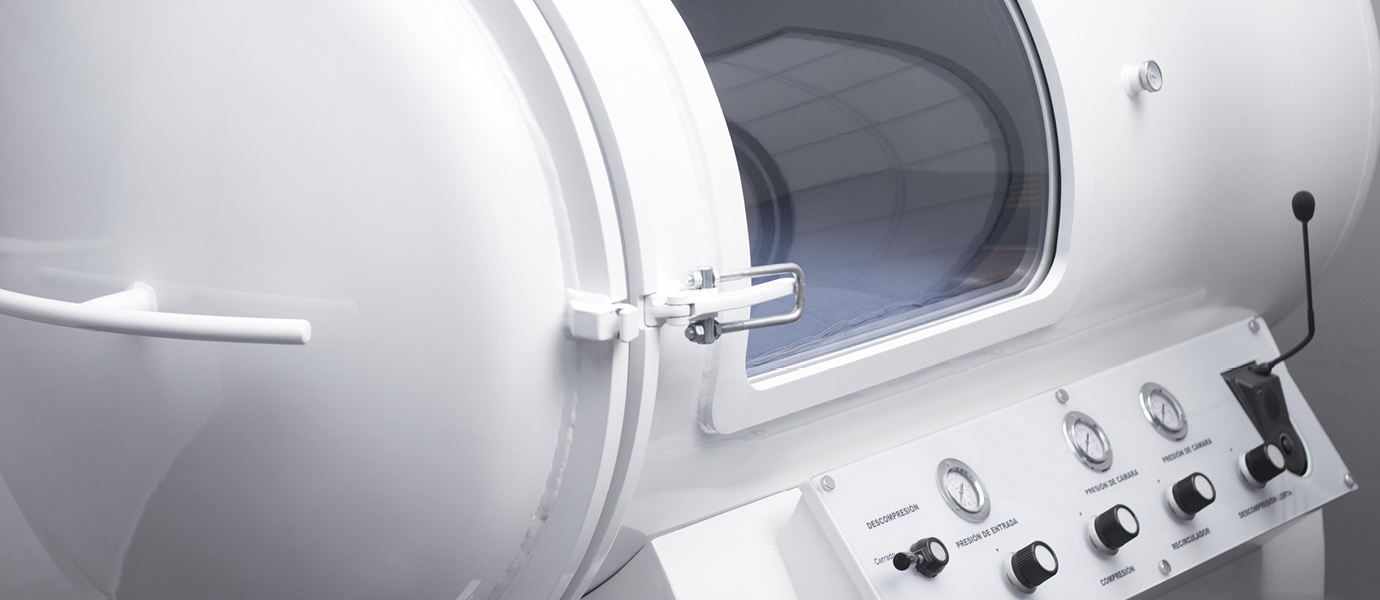
The OIG’s most recently published report reveals its findings of overpayments associated with HBO (and they’re not talking about the cable channel). Hyperbaric oxygen therapy (HBO therapy) involves giving a patient high concentration of oxygen within a pressurized chamber in which the patient intermittently breathes in 100-percent oxygen. A prior OIG review on HBO therapy expressed concerns that (1) Medicare beneficiaries received treatments for noncovered conditions, (2) medical documentation did not adequately support treatments, and (3) Medicare beneficiaries received more treatments than what was considered medically necessary.
More recently, a review by a Centers for Medicare & Medicaid Services (CMS) contractor found that claims for HBO therapy services were denied because of a lack of medical documentation to support that the services were medically reasonable and necessary. From 2015 through 2018, CMS conducted a prior authorization demonstration program for non-emergent HBO therapy in Illinois, Michigan, and New Jersey. The program did not create additional documentation requirements but required the documentation to be submitted earlier in the claim payment process for certain covered conditions. CMS is using this program to test whether prior authorization reduces expenditures while maintaining or improving quality of care and ensures HBO therapy services provided are in compliance with Medicare requirements. The results of this pilot have not yet been made public.
For this most recently published review, the OIG focused on one Medicare administrative contractor (MAC), First Coast Service Options, Inc. (First Coast), because of all MACs, it paid the second largest amount for HBO outpatient therapy services in 2013 and 2014. During the same time period, Wisconsin Physician Services paid the most for HBO outpatient therapy services but has already been audited by the OIG.
Medicare Part B covers hospital outpatient services including HBO therapy. CMS administers the Medicare program. CMS issues National Coverage Determinations (NCDs) that indicate whether a particular service is covered. NCD 20.29 allows Medicare coverage for HBO therapy. It states, “For purposes of coverage under Medicare, HBO therapy is a modality in which the entire body is exposed to oxygen under increased atmospheric pressure.” Medicare reimbursement for HBO therapy is limited to that administered in a chamber and only for 15 conditions, including diabetic wounds of the lower extremities and chronic refractory osteomyelitis (chronic bone infections).
For diabetic wounds of lower extremities to be covered by Medicare, documentation in the patient’s records must support that the patient has (1) type I or type II diabetes and has a lower extremity wound that is due to diabetes, (2) a wound classified as Wagner grade III or higher, and (3) failed an adequate course of standard wound therapy. HBO therapy is covered as adjunctive therapy for diabetic wounds of lower extremities only after there are no measurable signs of healing for at least 30 days of treatment with standard wound therapy and must be used in addition to standard wound care (NCD 20.29).
The documentation for patients with chronic refractory osteomyelitis must support that the condition was unresponsive to both conventional medical and surgical management. First Coast issued the Local Coverage Determination (LCD) L28887 on December 30, 2013, with an effective date until September 30, 2015. The LCD contains covered conditions relating to NCD 20.29. The LCD also contains noncovered conditions that should not be reimbursed by Medicare, documentation maintenance requirements for HBO claims, and diagnosis codes that should be billed for rendering the HBO service under the covered conditions.
During CYs 2012, 2013, and 2014, hospitals billed Medicare for outpatient HBO therapy services using Healthcare Common Procedure Coding System (HCPCS) code C1300, hyperbaric oxygen under pressure, full body chamber, one unit for each 30-minute interval. Effective January 1, 2015, HCPCS code C1300 was discontinued and replaced with HCPCS code G0277.
Of the 120 sampled outpatient claims totaling $415,513, First Coast made payments for HBO therapy in accordance with Medicare requirements for 5 claims. However, First Coast made payments for HBO therapy that did not comply with Medicare requirements for 110 claims (92 percent), resulting in overpayments for HBO therapy totaling $351,970. OIG did not review the remaining five claims because one was canceled and the Recovery Audit Contractors (RAC) indicated that the other four were under review by another entity. First Coast made payments for HBO therapy that did not always comply with Medicare requirements because First Coast had limited policies and procedures in place to ensure it made correct payments. During the audit period, First Coast did not have effective automated Medicare Part A prepayment edits in its claims processing system to monitor HBO therapy coverage. Based on OIG’s sample results, they estimated that First Coast overpaid providers in Jurisdiction N $39.7 million during the audit period for HBO therapy that did not comply with Medicare requirements.
Examples of failure to meet the requirements included:
Example 1: A Medicare beneficiary underwent seven HBO therapy sessions as of 4/25/2014, for treatment of osteomyelitis. HBO therapy for osteomyelitis can be a Medicare-covered condition when it is chronic refractory osteomyelitis and has been unresponsive to conventional medical and surgical treatment. The medical records indicated that HBO therapy treatment began before the conventional treatment had been completed. The hospital billed $1,949 for these six HBO therapy sessions.
Example 2: A Medicare beneficiary underwent 35 HBO therapy sessions as of 11/30/2013, for treatment of a failed flap procedure, which is a covered condition. However, there was no evidence that the beneficiary ever received a flap procedure. She had surgery that resulted in a wound that became infected and did not heal, but there was no evidence that she ever received a flap. The hospital billed $7,604 for 24 of these HBO sessions.
Example 3: A Medicare beneficiary underwent 58 HBO therapy sessions as of 10/11/2013, for treatment of a diabetic ulcer, which can be a covered condition when at least 30 days of standard wound care therapy are provided, with no measurable signs of healing, prior to HBO therapy. However, the medical records did not contain sufficient documentation to support that there were at least 30 days of standard wound care therapy provided prior to HBO therapy. The hospital billed $2,535 for eight of these HBO sessions.
The OIG Recommended That First Coast:
- Recover the portion of the $351,970 in Medicare overpayments from the 48 providers for the 110 incorrectly billed claims that are within the 4-year reopening period.
- Notify the 70 providers responsible for the remaining 46,737 non-sampled claims with potential overpayments estimated at $39.3 million so that those providers can exercise reasonable diligence to investigate and return any identified overpayments, in accordance with the 60-day rule, and identify and track any returned overpayments as having been made in accordance with this recommendation.
- Identify and recover any improper payments for HBO therapy services made after the audit period.
- Work with CMS to the extent possible in developing more effective automated HBO therapy prepayment edits in the claim processing system, which would result in millions of dollars in future cost savings.

Questions or Comments?