Episode 79:
Research Realities: Insights into Clinical Trials
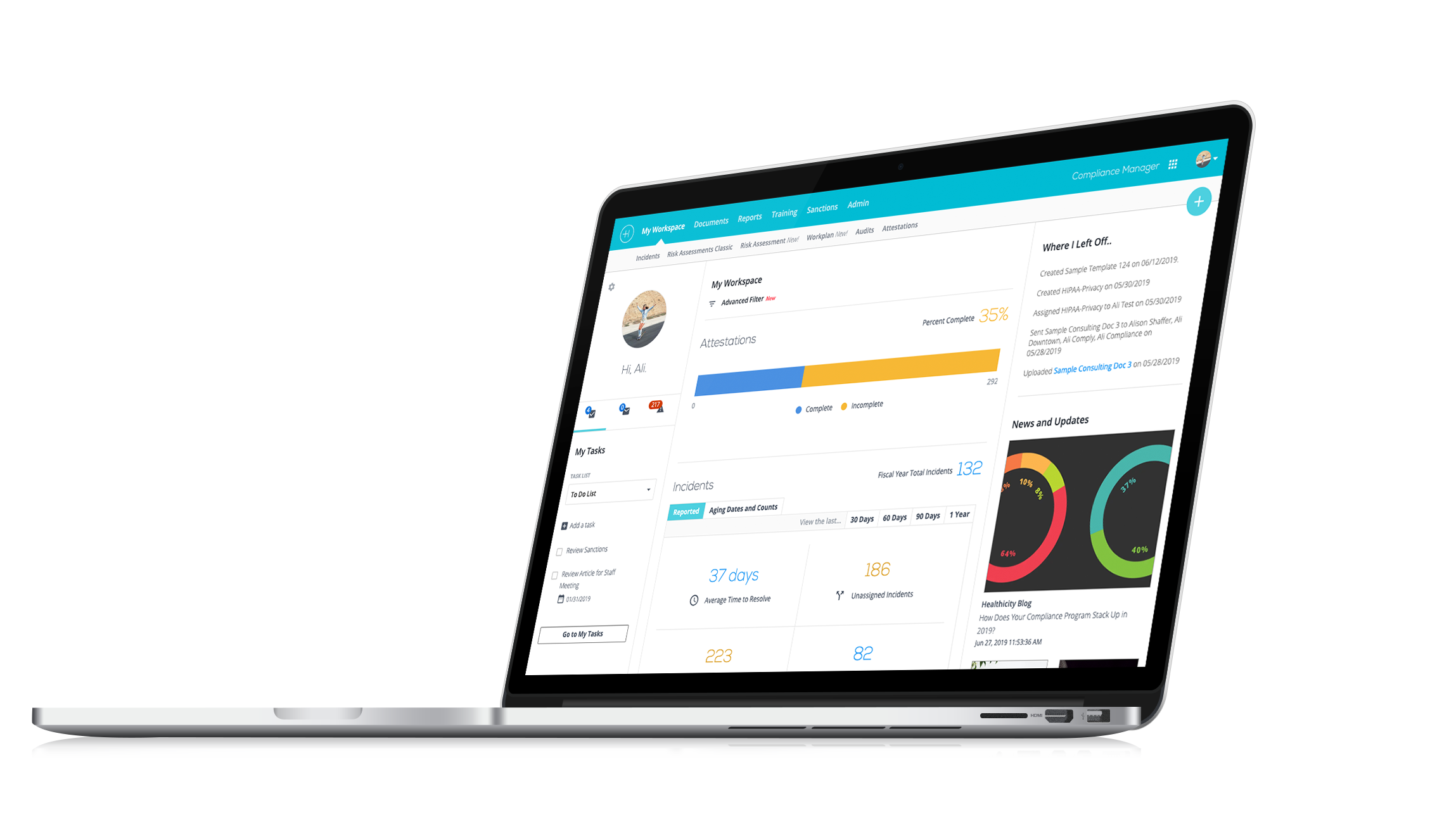
Watch the demo:
Compliance Manager
See the only all-in-one compliance solution today.
Dive into the world of clinical trials compliance with Jenny Hamilton as she shares valuable insights on FDA audits, informed consent nuances, and the global impact of cutting-edge medical research in our latest podcast episode.
In this episode, Jenny Hamilton the Clinical Project Research Manager at Barrow Neurologic Institute, joins CJ Wolf, MD for an in-depth discussion on compliance considerations for clinical trials.
From the complexities of protocol deviations to the vital role of Institutional Review Boards, they cover a wide range of topics. Tune in for valuable insights into the compliance landscape of clinical trials and learn more about the crucial role patients play in advancing medical research.
Jenny and CJ also cover:
-
- The importance of informed consent in clinical trials
- Insights into FDA audits and the role of Clinical Research Associates
- The fascinating and diverse landscape of global clinical trials
You can also learn more about Jenny’s work here.
Interested in being a guest on the show? Email CJ directly here.
Episode Transcript
CJ: Welcome everybody to another episode of Compliance Conversations. My name is CJ Wolf with healthicity and today our guest is Jenny Hamilton. Welcome, Jenny.
Jenny: Hi, CJ, how are you?
CJ: I'm doing great. Thank you so much for joining us today. Our guest today, everybody has a lot of experience and expertise in clinical trials research. And so, I know that is an important topic in compliance and she's going to share some good insights, I think. But Jenny, before we kind of jump into that topic, we'd like to just hear from you a little bit. Tell us a little bit about yourself. How did you get involved in what you're doing and a little bit about your professional life.
Jenny: Sure! Thanks so much for having me on. I'm a clinical research project manager at Barrow Neurologic Institute in Phoenix, AZ, which is one of the top neurological treatment and research facilities in the country and in my role, I oversee the training and certifications of clinicians and research staff who perform specialized clinical assessments on patients with amyotrophic lateral sclerosis, better known as ALS or Lou Gehrig's disease. We work on over 20 pharma industry trials and our training has trained and certified 1200 clinicians and staff in over 30 countries, so we're a busy group.
A little bit on my background, I started out in clinical research and as a data manager and a study coordinator on phase one oncology trials, which is definitely kind of hitting the refiners fire stuck out because those are typically some of the more intense trials and they are higher risk for FDA audit. And my career took a little bit different turn for a couple of years where I managed or I was a project manager on a marriage and family therapy study at an academic Research Center. And then during COVID, I was a clinic coordinator for a medical device study. And I got the opportunity to write several research protocols while our research operations were shut down so that was an interesting time in clinical research because a lot of things went on pause.
But I got my start in healthcare, I was a volunteer in quality management at a big hospital in Portland, OR and that was a really unique opportunity to see risk management up close. And you know, one of my favorite things was I got to shadow the hospital leadership during a Joint Commission survey so that.
CJ: Right!
Jenny: That was really an interesting experience and I think it was, you know, it was really good to give me a good overview of what really happens in the hospital environment.
CJ: Exactly! Well, that's an exciting background and a lot of great experience. And I hear you when you said, you know, on the oncology stuff. So, I spent some years at MD Anderson Cancer Center, though I wasn't directly over the clinical part of the clinical trials I was involved in kind of the research billing and that sort of thing, but I hear what you're saying with, you know, the importance of those types of trials, you know, in just in general before we get into kind of the compliance side of things. I'm interested if you have any thoughts, but I'll share some first on just the importance of clinical research. You know, most of us take advantage of these advances in medical technology and in in drugs and treatment and a lot of that, you know, it comes from people who are willing to enroll in clinical trials, sponsors who are willing to sponsor the research, but it makes a huge difference in in the lives of individuals. And I bet you're seeing that on a daily basis.
Do you have any general thoughts just about the importance of clinical trials and that work in general?
Jenny: Yeah, it's such an important work and you know, working in ALS research is has been eye opening because I think through about 2011 there were only two treatments available for ALS, and they just added a couple of months to life expectancy and just in the past several years we've had actually in the last year we've had two drugs approved. So, you know it's giving a little bit of hope and it's just amazing to see the leaps that medical technology is taking through clinical research.
CJ: Absolutely! And because it's so important, and because the decisions that are made either by regulatory bodies or clinicians rely on, you know, the excellence of the trial, how it's set up, you know compliance to the protocol, making sure patients are safe, there's a lot of safeguards, a lot of processes in place to make sure it's done right, and so maybe we can start there is can you just share, just a general oversight of who's providing oversight on clinical trials? There's lots of different parties involved, but you know, kind of big picture for those. You know, we have a lot of compliance folks listening and some of them have experience and research and some of them might not. But who are the big players in oversight?
Jenny: Yeah! The FDA, of course, all clinical research trials have to be approved by the FDA before anything gets started as far as that. Of course, we also have...
CJ: Like the IRB is one like so and I apologize, I probably should have said, you know there's external, but then there's also kind of internal and we'll get to a little bit of that, but sorry. Go ahead. If there's anything else.
Jenny: Oh, yeah, no worries. No worries. Yeah, it's we are. We are mindful of, you know, the FDA, IRBs have a lot of say in what we do at the institutional level and you know there are times that we go back and forth with the sponsor quite a bit on even just the protocol. With different language for the site, you know we work on International Studies. So, we're also working with the European FDA version of that. So, and then we're of course we're governed by institution guidelines and lots of, you know, international guidelines and just documents for that give guidance for ethical research.
CJ: Got you. Yeah, absolutely. All these different players, right? External internal guidelines like you said, sponsors, partners, all really, really important. So maybe we start there with the FDA. You know, when I was working in an academic medical center, there were times that FDA would do audits and I'm kind of curious if you've ever been through an FDA audit, you know, what did you learn? What are they looking at when they come in or anything involved with kind of FDA audits?
Jenny: Oh, sure! My first year in research we were on an oncology trial. We did go through an FDA audit. One of the interesting things as you may or may not get notification that the FDA is going to be on your doorstep. So, in the instance of our audit, we got a call Friday at noon and they were on our doorstep Monday first thing.
CJ: Oh boy!
Jenny: So yeah, so there's a lot of scrambling, a lot of long hours over the weekend as you're trying to pull together the documentation, make sure everything's in order, just so that you're ready to do that. And you know, as they go through, they'll be reviewing specific subjects. They really focus on informed consent. And subject eligibility training is a huge piece of what they look at because you know one of the requirements is that everyone is qualified by education, experience and training to be doing their roles and that they are only performing those roles that the site investigator has delegated authority to.
CJ: Got you.
Jenny: And then they, of course, they look heavily at safety. So adverse events, serious adverse events, just making sure that protocols being followed and that patients are safe.
CJ: Yeah! Are there certain risk factors that might prompt an audit, that are more likely to prompt an audit than others? Or is it certain types of trials or anything in that regard that you're aware of?
Jenny: Yeah, as I mentioned, you know, working on phase one studies, they are higher risk for FDA audits just because that is the first time that many drugs are being given to patients and so that is an important part. They also when they're looking at which sites to go to because there may be dozens of sites working on a study, they will look at sites that are high in rolling.
And you can usually expect an audit around the time that a drug is anticipated to go up for approval, for marketing with the FDA, they will typically choose some sites to go for that and then if they ever get a complaint from a patient or anyone that goes directly to the FDA, then they will go and look into that further.
CJ: And you know you're mentioning sites and so just for the folks that and you can correct me if I'm wrong, for the folks who might not be as familiar with the details, the clinical trial you know might be you know it's looking at a certain variable of a disease process or a drug or medical device and the protocols written, but you're enrolling people in all sorts of different sites, if available, right because you're trying to maximize enrolment. And so, you might have a site in one state and another site in another state. And so, when you're referring to kind of those high-end rolling sites, it's the sites where there's more people entering into the clinical trial, is that right?
Jenny: Exactly! And you know, there are institutions that have large research programs and they have the staff and the bandwidth to take on a lot of patients and they might be more central centres that people look to, you know, for example, like Mayo Clinic would be at that type of site.
CJ: Yeah, you mentioned informed consent. Can you just, you know, we talk about in, in healthcare, we know we talk about informed consent all the time, right? Like if I'm going to get a surgery done, the doctor will describe, "OK, here are the risks here are the benefits, here are the risks if you don't do the surgery," and then you sign a piece of paper usually. How is that different in research?
Jenny: It is a very different process in research to be sure. You know, I remember when I had to have an emergency appendectomy and I'm signing the informed consent form as I'm being wheeled down the Gurney down the surgery and that type of thing is not typically going to happen in clinical research.
CJ: Right!
Jenny: There is a big emphasis on when we're doing informed consent with patient on something called the therapeutic misconception. Which is, you know, these clinical trials are research. We're testing a new drug and trying to get information about it. And the odds are that the patient is going to have minimal benefit from it. We always hope and pray that they're going to benefit from it, but we need to be very clear with the patients up front, this is research and this is science and this is more of a service than for them to expect to benefit from.
They have to sign consent before any study visits are done. They should be given it ahead of time to review and just discuss with family, and then usually the physician will go over the consent with the patient which has the risks and the benefits and it has information on where they would go if they have any questions or concerns or and it describes what happens if heaven forbid, they're injured during the trial.
So, there's a lot more information and we just have to be very, very careful to discuss it very carefully with them and to document that and then anytime the protocol is updated, the patients have to be reconsidered. So that that could be tricky.
CJ: Yeah! So, my understanding is that the informed consent will be different for every trial, right? Like in the hospital, it's like, you know, you might have some sort of template that the doctor fills out risks and benefits, it's the same form for any kind of surgery, maybe, but in clinical trials it's specific to that trial. What's being tested, you know, if you're in, you might be in a blinded study where you might not get the medication or the medicine. And so, you have to recognize that. And if you're being obviously being treated for a disease, then you might not be getting any, you know, therapeutic benefit from the drug like you were saying. And so, you have to be specific, right? And the informed consent, as you mentioned has to be updated if any of those things change for that trial.
Jenny: Yeah, for sure. And usually, the sponsors will send an informed consent to the sites, but it has to go through IRB approval. And sometimes that has to be adapted. So, I've worked at Catholic institutions and so they're, you know, different issues with, for example; birth control where the consents have to be adjusted per the institution to fit those requirements.
CJ: Well, this is great! Let's take a short break and then when we come back, I want to maybe start talking about the IRB a little bit. So, stay with us everybody, we'll be right back.
Welcome back everybody! We are here with Jenny Hamilton. She's telling us all about clinical trial research and some of the regulations and oversight that that goes on. And we were talking about informed consent and she mentioned that, you know, those documents have to be individually approved by the IRB. Jenny, tell us what an IRB is first and then maybe just kind of the role that it plays.
Jenny: Sure! So, an IRB is an institutional research board. Every institution will have one. Sometimes they are affiliated with the institution, other times, some studies are starting to use central IRBs. But their role is to make sure that the research is conducted in a way that protects patients. And that follows the institutional guidelines.
It's made-up of both physicians and there will usually be a just average citizen type of member on it and every protocol, every consent form, every document that will be used in the trial will go through the IRB and has to be officially approved. And that even includes information that's given to patients. So, if a site thinks that, "Oh, it would be helpful to have this little, you know, explanation guide for the patient," that actually has to go through the IRB and be officially approved in order to share that with the patient.
CJ: That's really helpful. And the you mentioned the types of things they approve, like, the protocol, the informed consent. Do they ever deal with, so like if and we're going to talk a little bit more about deviations in a second, but do they deal with things during the trial as well? or is it mostly like; "No, this is all these are all the steps that have to be done before you can begin the trial that goes through IRB." Are they involved in anything during and then after?
Jenny: Yeah, absolutely. They will monitor protocol deviations. They will also want to be informed of serious adverse events, particularly if it's something that is related to the drug but was not expected side effect. They're going to be involved throughout the trial and they are providing a heavy level of oversight at the institutional level and they will be involved also as the study is closed. If for some reason the study is ended ahead of what is expected, they will need to be informed as well.
CJ: So, you mentioned protocol deviations, can you tell us just what is a protocol first of all and then maybe describe a little bit about deviations and how they might be handled?
Jenny: So, protocol is basically the instructions for the study. It's also going to include the scientific background and reason for conducting the study, but it's going to contain all the information about when visits are to be conducted, what tests are required at what point in the study, they're also going to include instructions if there's, you know, with cancer drugs where you're having infusions, if there's an infusion reaction that occurs while the medication is being dosed. And then it's going to also explain how the data is going to be handled and analyzed on the back end.
So, it's a very comprehensive document. You know, when you're involved in the actual clinic operations, you're mostly focused on, you know, all of the instructions and of what to do with the visits and they can be quite complex. They can be, you know, maybe 10 pages. I've worked on protocols that are over 600 pages.
CJ: Wow! How do you keep track of that? I mean, that's got to be hard.
Jenny: Yeah! And then anytime the protocol is updated you have to be trained on it initially and then every time it's updated, you have to be trained on it again. So, that it's printing out a new copy to track the new changes.
CJ: Yeah! So a lot of trials, you have people who are really in the know on the protocol and then you probably have people who are like if a patient is coming through and maybe they're getting a CT scan or they're getting an infusion like are kind of frontline nurses and other personnel taking care of patients and they might not be as knowledgeable about the details of the protocol or tell us a little bit about that, about who the patient or the subject, the enrolee would be interacting with, I'm sure it can probably vary.
Jenny: Yeah! It does when we were in oncology, obviously that they're going to go to the infusion clinic to receive the drug and those nurses are not going to be familiar with the protocol. And that's where the role of a research coordinator or a research nurse is very important because we will communicate that information to the nurse so that they are aware of what the drug they're giving? What tests and vitals and whatnot they need to be taking throughout, I mean, so there's really close communication so that they understand what we need from them, but they don't have to be, you know officially trained on the protocols typically.
CJ: So that nurse coordinator, because I'm what I'm getting at is how do people know when there is a protocol deviation? Like if I'm a frontline nurse, I'm right and I'm not intimately aware of all the details of a 600-page document, how do I know if the protocol has been deviated? Are people doing audits? Like, do you see what I'm saying, how was brought up and identified?
Jenny: Yeah! So, deviations aren't typically don't usually get noticed at the time, because a lot of them will be like, you know, take a blood pressure one hour after the infusion ±5 minutes, and so if they do it at 7 minutes after the hour, that's a deviation. But then we have every study has monitors that sponsors typically contract with organizations that provide monitoring services and so they come through usually about every month or so and they review data, they look at things that have been happening with the trial to make sure that we're following all of the protocol requirements. And so, if they find any discrepancies, then they will bring that to the attention of the coordinator and then we'll work on either providing the explanation, providing the correction, or if there's more action.
CJ: So that's kind of what's known as a site monitoring visit, it's more of not you correct me if I'm wrong, it's not necessarily like an external agency, we already talked about an FDA audit, but it's more of like an internal like the sponsor or somebody hires or has people to just monitor compliance with the protocol, is that right?
Jenny: Yeah! They're known as Clinical Research Associates and they are specially trained to go in and to look at all of the information and make sure that the study is being conducted, you know, the way that it's supposed to that data is being, you know, collected appropriately and recorded appropriately.
CJ: Are there, and if there aren't just let me know, are there certifications for people in the realm of clinical trials? You said you're a clinical research coordinator. There’re probably people who audit and do that sort of thing. Are you aware of those types of certifications?
Jenny: Yeah! I'm a certified clinical research coordinator. There're two organizations that provide certifications in clinical research. One is ACRP and the other is SOCRA. And they both provide certifications for people that work on clinical trials. They provide them for coordinators for the Clinical Research Associates, even site investigators can receive certifications for working on clinical trials. It's not something that's required, but you know there it is often requested when you're applying for jobs that they're looking for that.
CJ: Yeah! Now that makes a lot of sense. And on the on the general compliance side, so those of you who are listening that are familiar with the Healthcare Compliance Association, there's also a certification called certified in Healthcare Research Compliance. It's different than what Jenny's talking about it's more; are you familiar with things like clinical research billing? Are you familiar with privacy standards, HIPAA, and what trumps what in the data privacy and research, IACUC which is, you know if there's animal type of involvement in studies and those sorts of things. So that sounds like probably a little different than these very specific certifications that you're referring to.
Jenny: Yeah! These certifications are based on ICHGCP of the international governing documents, also FDA regulations. So, they're really testing to see if you have an in-depth knowledge of what the requirements are.
CJ: Yeah, that's awesome. We're getting kind of towards the end. I want to mention one other thing and then also see if you have comments on this as well as any kind of closing comments. So, I have had family members who have had certain conditions where we want to look for a trial. So, I've always gone to clinicaltrials.gov, which is a website where I think almost all clinical trials are kind of registered, there may be some exceptions there, but you can search by location. You can search by disease type; you can search by intervention. Are you familiar with that site and do you have any thoughts about it?
Jenny: Yeah, that is a great site and that is the number one place to go to look if you're looking for a clinical trial and then if you're near an academic medical centre, you can reach out to them as well. But a lot of times they're going to point you at the clinicaltrials.gov it's a great place to start.
CJ: Yeah, and like it'll list out a lot of the information it'll tell you, "I don't think the whole protocols on there," but you it'll list out a summary of this is what we're studying, you know, Group A will be randomized to this arm, Group B with this arm or whatever. So, you can really learn a little bit more about that. And then, like I said, you can usually find the sites that are enrolling. You know some trials are on there and it says, "Oh, we're done enrolling and we're in the middle of the trial," and so you can kind of get a sense of where things are.
Plus, if you're just interested in learning academically about what's going on, you know, sometimes people wait until things get published in the medical literature, which is a good place, right? Because the stuff has to withstand kind of peer review but clinicaltrials.gov is a great place just to kind of see what's going on in the field and what people are researching. And I think it's fascinating.
Jenny: It really is and there's so many new amazing, you know, with stem cell therapies and gene therapies and immunotherapies, there're so many new breakthroughs in in medicine and it's exciting to see what's on the horizon.
CJ: Yeah! And it's both drugs and devices and it's not just always like cancer, obviously is a really important area, but like even depression and behavioral health and there's trials now on psychedelics and you know, it's just a scientific playground and I shouldn't say it that way! It's not a playground but it's scientific community exploring what can be done in the field of science and I just think it's wonderful.
Jenny: That's great!
CJ: Jenny, this has been so amazing. Are any last-minute thoughts or comments, things that I didn't ask that you think people might need to know about when it comes to research compliance and those sorts of things.
Jenny: You know, this has been a great discussion. I really appreciate the opportunity to talk about clinical research because it is such an important part of the medical world. You know, I really respect the patients that sign up for these clinical trials. Because they're doing something really selfless in participating because they know that they may never get benefit from this. But they know that they're contributing to the body of knowledge. We've had a couple of ALS trials stop because the drugs were deemed not having any effect or any impact on the disease and those are tough days in research, but yet it teaches us, "OK, let's not go down that path any more. Let's look at different paths." So, whether its trial is successful or not, it's really important knowledge that goes into developing treatments and hopefully one day we'll get to the end of cancer. And you know, the ALS patients will have good treatments that will prolong their lives and give them good quality of life. So, it's an important work to be involved in and I really appreciate the patients who sign up and take part in these.
CJ: Yeah, I completely echo that. On that note, historically, a lot of research has been done on white males and there's a lot of effort over the last many, many years and into the future of getting a more diverse kind of patient background and demographic, there's a lot of international excitement right in getting trials done in places that normally have not been done. So, for example, in Africa and there's some places that are really booming with clinical research because it's important cause different genetic makeup might respond differently. You know, gender might respond differently. And so, in enrolling people from a diverse background is really important. And you've probably seen that too, right?
Jenny: Yeah! And we work it on studies in over 30 countries and in recent years there's a push to kind of bring our research together now that it's more of an international experience and to bring together all the different efforts. We're we work with sites in China, in Japan, in Israel, Ukraine, Russia, Turkey, it's really exciting to see all the places where clinical research is going.
CJ: Yeah, I was on a site the other day that was the main registry for clinical trials in the continent of Africa and was just fascinated by what the work being done there as well. So exciting times!
Jenny: Yeah, definitely!
CJ: Well, Jenny, thank you so much for being willing to share your time today and to share your expertise. We really, really appreciate it.
Jenny: Well, thank you. I appreciate the opportunity to be on. You're doing great.
CJ: Well, yeah, thank you so much. And thanks everybody for listening to another episode. If you're liking these episodes, please share with friends, subscribe and spread the word. And as always, I invite you to reach out to me if you know of a guest or a topic that you'd like to have covered. And until then, be safe, everybody. Thanks for listening!