Deeper Than the Headlines: Medicaid Fraud Control Units in 2018

compliance, OIG, deeper than the headlines, healthcare fraud, medicaid billing fraud, fraud, Medicaid Fraud, Medicare Fraud Strike Force, Medicaid Fraud Control Units, OIG annual report, fraud takedown, Medicaid Fraud and Abuse, Personal Care Services
Riddle me this: Who had 1503 convictions, 810 civil settlements and judgments, 973 excluded individuals or entities, and recovered $859 Million (at a rate of $2.92 recovered for every $1 spent)? The answer: The collective work of the Medicaid Fraud Control Units in the fiscal year 2018. Aren’t they incredible?
The OIG recently released the annual report of the Medicaid Fraud Control Units for the fiscal year 2018 and those headlining numbers are pretty significant.
The function of Medicaid Fraud Control Units (MFCUs or Units) is to investigate and prosecute Medicaid provider fraud and patient abuse or neglect. The Social Security Act (SSA) requires each State to effectively operate a MFCU, unless the Secretary of Health and Human Services determines that (1) the operation of a Unit would not be cost-effective because minimal Medicaid fraud exists in a State and (2) the State has other adequate safeguards to protect beneficiaries from abuse or neglect. Forty-nine States and the District of Columbia operated MFCUs in fiscal year (FY) 2018. In December 2018, OIG certified two additional MFCUs in the territories of Puerto Rico and the U.S. Virgin Islands.
MFCUs are funded jointly by Federal and State Governments. Each of the 50 MFCUs that was operating in FY 2018 received Federal reimbursement equivalent to 75 percent of its total expenditures, with State funds contributing the remaining 25 percent.
MFCU cases typically begin as referrals from external sources or are generated internally from data mining. MFCU staff review referrals of possible fraud and patient abuse or neglect to determine the potential for criminal prosecution and/or civil action. If the Unit accepts a referral for investigation, the case may result in various possible outcomes. Criminal prosecutions may result in convictions; civil actions may result in civil settlements or judgments. Both criminal prosecutions and civil actions may include the assessment of monetary recoveries.
The Office of Inspector General (OIG) has the authority to exclude convicted individuals and entities from any federally funded health care program based on convictions referred from MFCUs. In addition to achieving these case outcomes, Units may also make program recommendations to their respective State Governments that help strengthen program integrity and efforts to fight patient abuse or neglect.
Personal Care Services (PCS)
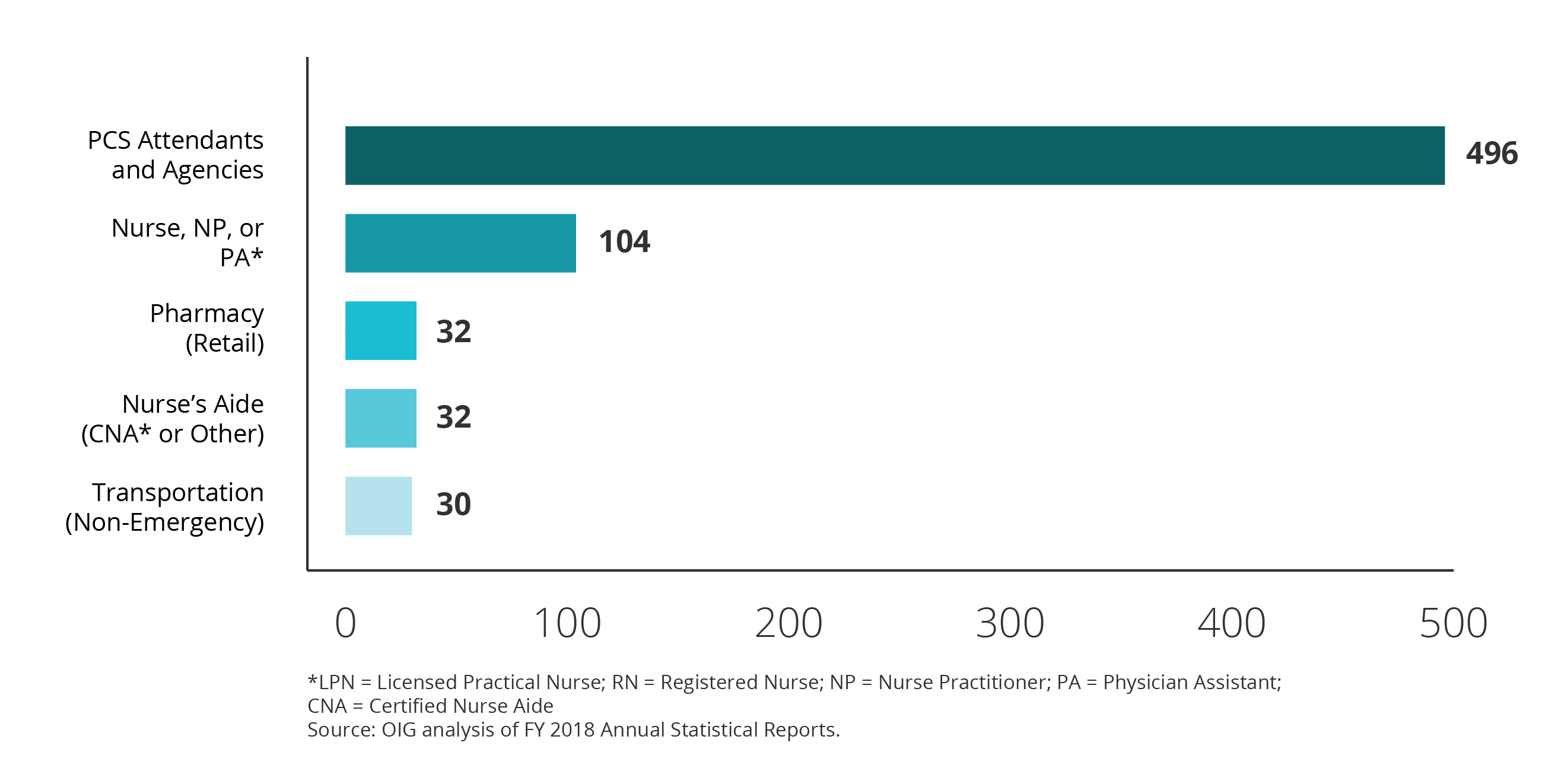
In FY 2018, there were significantly more convictions for fraud involving personal care services (PCS) attendants and agencies than any other provider type. Of the 1,109 fraud convictions in FY 2018, 496 (45 percent) involved PCS attendants and agencies.
Convictions from Drug Diversion Cases Continued to Increase
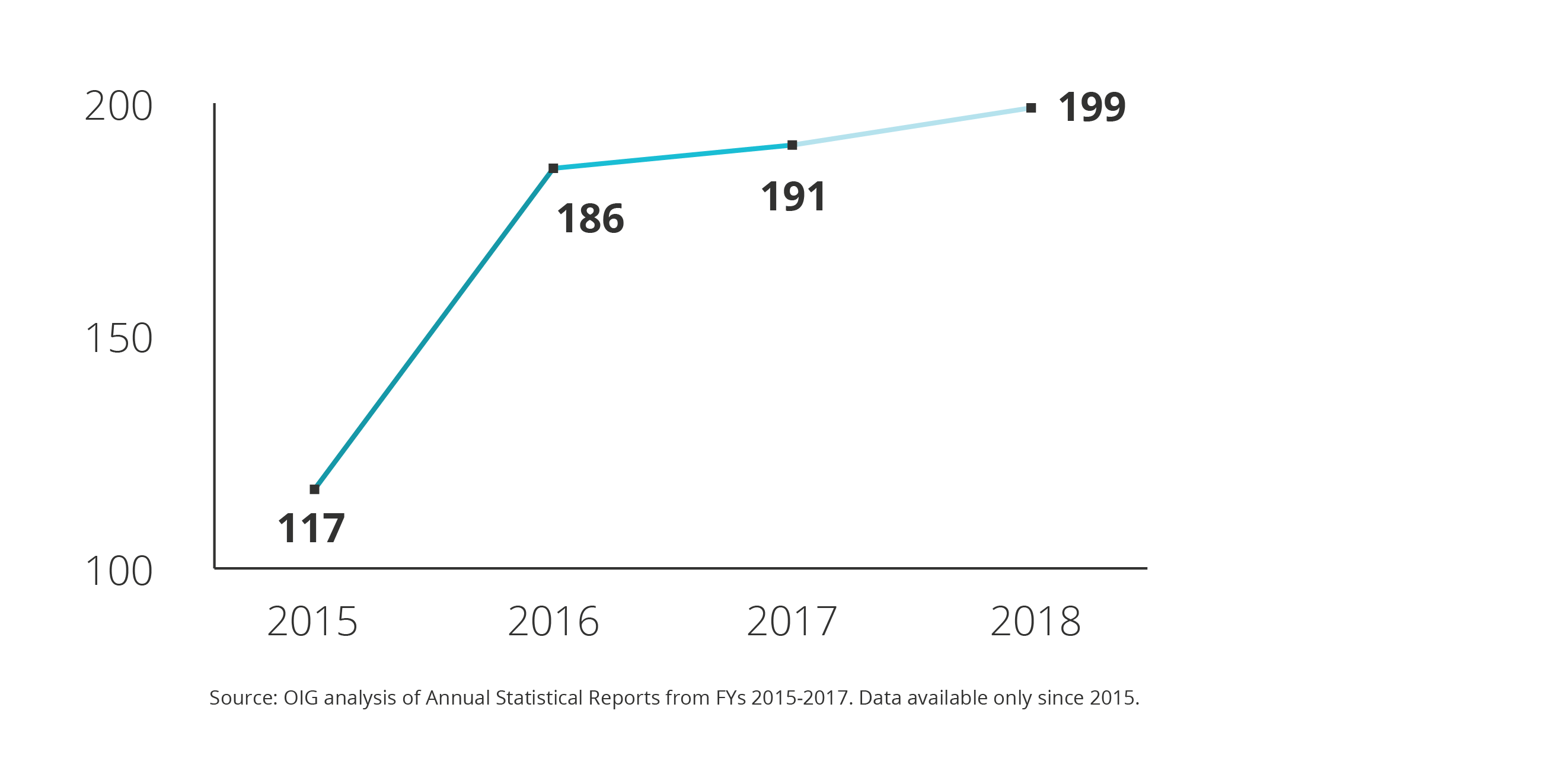
Convictions from drug diversion cases increased from 191 in FY 2017 to 199 in FY 2018, with associated recoveries of $7.7 million in FY 2018. In a Medicaid context, drug diversion cases involve investigating the fraudulent billing of Medicaid for drugs diverted from legal and medically necessary uses. MFCUs may conduct drug diversion investigations jointly with other State or Federal agencies, such as OIG or the U.S. Drug Enforcement Administration. The graph below shows the number of convictions associated with drug diversion cases during FYs 2015 through 2018.
Patient Abuse
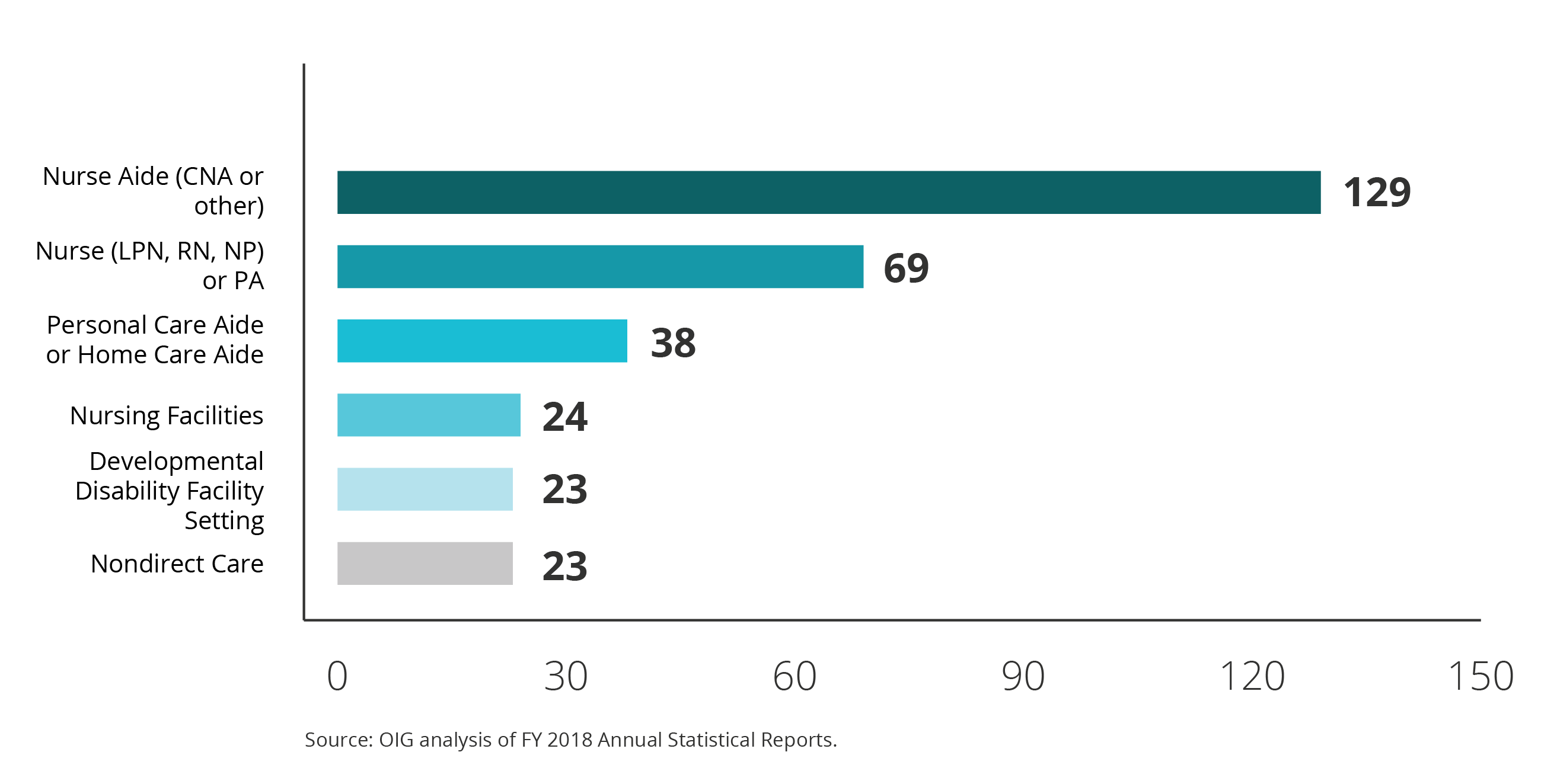
In FY 2018, more convictions for patient abuse or neglect involved nurse aides than any other provider type. Nurse aides accounted for 129 of the total 394 convictions for patient abuse or neglect (33 percent). The exhibit below shows the provider types with the most convictions for patient abuse or neglect.
Settlements with Pharmaceutical Manufacturers
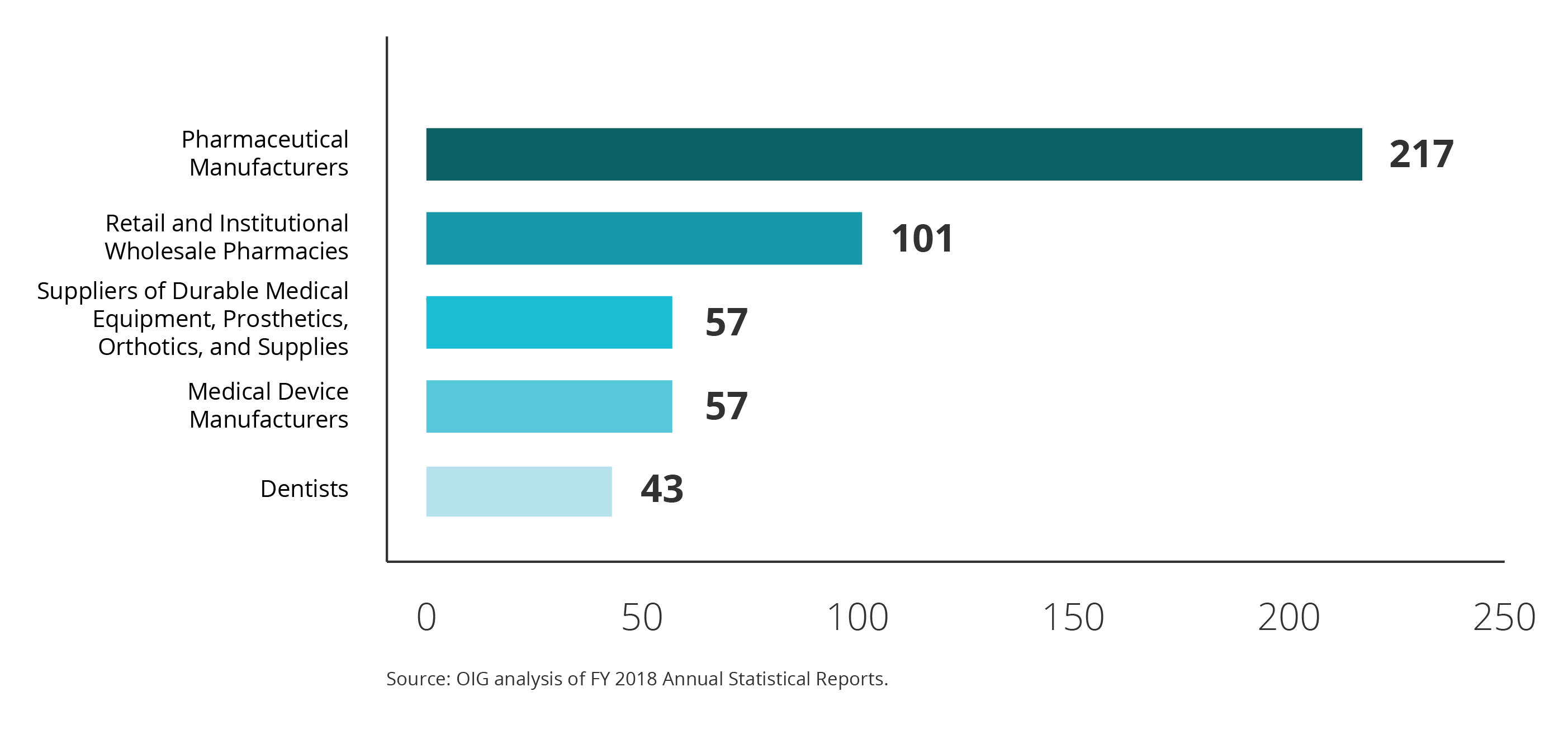
Significantly more civil settlements and judgments involved pharmaceutical manufacturers than any other provider type. Of the 810 civil settlements and judgments in FY 2018, 217 (27 percent) involved pharmaceutical manufacturers. The graph below shows the provider types with the most civil settlements and judgments in FY 2018.
Other Examples
The report also mentioned a couple of other examples of cases.
As a result of one case, a dental management company and its affiliated dental clinics were ordered to pay the United States and participating States a total of $23.9 million. This was to resolve allegations that the company and its affiliated clinics had knowingly submitted false claims for payment to State Medicaid programs for medically unnecessary dental services performed on children insured by Medicaid.
In another case, the Alaska Unit investigated a health care agency that provides services to persons with intellectual or developmental disabilities. That agency agreed to pay $2.3 million to resolve allegations that it billed for services not provided. As part of the settlement agreement, the provider was also required to enter into a 5-year Corporate Integrity Agreement with OIG to help prevent future instances of fraud or abuse.
Conclusion
The appendices of the report are full of statistics and specific details of the providers who were investigated or settled. Knowing that the MFCUs are having much success in their efforts should tell all compliance officers that their efforts should also include a focus on Medicaid compliance and not just Medicare compliance.

Questions or Comments?