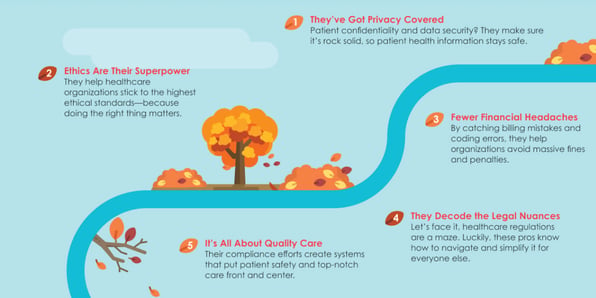
Thanksgiving is the perfect time to reflect on what—and who—we’re grateful for. This year, let’s give a big shoutout to the healthcare compliance and auditing professionals who work tirelessly behind the scenes to keep everything running smoothly.
Healthicity Blog
Subscribe for Healthcare News, Simplified.
Understanding How the DOJ Holds Individuals Accountable
Lessons from Compliance Communication and Leadership

In the latest episode of Compliance Conversations, CJ Wolf welcomes Jay Anstine back to explore the nuances of effective compliance communication.
Your Guide to Understanding RAC Audits

You’re invited to our upcoming webinar to talk all things RAC (Recovery Audit Contractor) audits – and how to optimize your audit responses and mitigate potential financial impacts.
Improve Audit Efficiency with Customizable Checklists
Preventing Improper Payments: Insights from the Field

In the latest episode of Compliance Conversations, CJ Wolf welcomes Nancy Clark, a seasoned expert in healthcare coding and revenue cycle management. Nancy shares insights from her extensive experience as the Senior Manager, Health Care Services as EisnerAmper, where she works to educate providers...
October OIG Updates: Key Areas to Watch
Deeper Than the Headlines: Alleged EGD Billing Missteps from Bariatric Surgeon

In a recent case, a general and bariatric surgeon agreed to pay $45,000 plus interest to resolve allegations related to improper billing practices involving esophagogastroduodenoscopies (EGDs) performed on bariatric patients. The settlement comes as part of an investigation by the U.S. Attorney’s...