Setting the Record Straight: Using the 2021 E/M Time Calculation

auditing, e/m coding, medicare, e/m audits, CMS, cpt, e/m services, CPT codes, MDM, HCPCS, outpatient services, AMA, e/m changes, Prolonged Codes, RVS, O/OO, Resource-Based Relative Value Scale
With the launch of the new E/M guidelines in January 2021, we now have two different Prolonged Codes to use. That’s a result of the different calculations defined by the American Medical Association (AMA) and the Centers for Medicare and Medicaid Services (CMS) Final Fee Schedule. While CPT® instructs us to use code 99417, CMS instructs us to use HCPCS code G2122.
This divergence has left many of us coders and auditors scratching our heads trying to understand the lingering questions and uncertainty around how to properly apply these guidelines. Does the AMA and CMS define total visit time differently? Do we use the total visit time or the usual time? When should we apply the CPT® code, and when should we apply the CMS code for prolonged times?
Before we can answer these questions and understand where we’re going, it’s important to understand where we have been. To do this, let’s go back in time.
Evolution of Time Associated with E/M Services
In 1992, the AMA began to include time as a factor to assist in selecting the most appropriate E/M level for office (and other outpatient) services, inpatient services, and consultations. The times listed in the CPT® code book was considered the average time a physician spends caring for a patient. This “average time” is often also referred to as “usual time,” or “typical time”.
This “average time” is not the same time we use for calculating the level of service or billing units. Rather, this average time is used to determine the value of a CPT® code, ultimately leading to the reimbursement of a code. To better understand the average time, and how the value of CPT® is determined, you must first understand a few acronyms. RUC is an acronym for the AMA and Specialty services Resource-Based Relative Value Scale (RVS) Update Committee. It is this committee that assigns the RUC-Value for the CPT® codes. This RUC-Value is then used to assign the Relative Value Units (RVUs) to the codes.
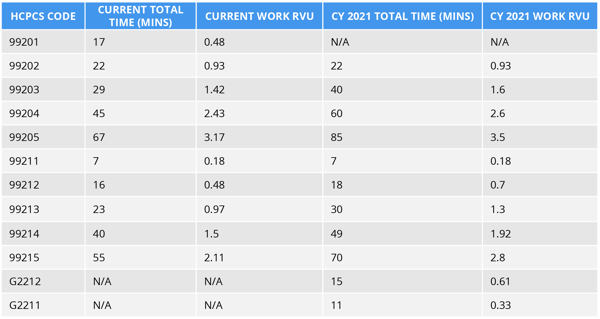
Now, let’s fast forward to the present. The AMA RUC committee resurveyed all Office and Other Outpatient (O/OO) E/M services concurrent with the CPT® Editorial Panel, redefined the average times a physician spends caring for a patient. They provided CMS with recommendations for the RUC-Values. Likewise, CMS addressed and responded to these recommendations and finalize new values for the CPT® codes 99202 through 99215. These values are listed in the Final Physician Fee Schedule release December 2, 2021. Below is a table with the new “usual” times and RVUs.
Table 20: Summary of Codes and Work RVUs Finalized in the CY 2020 PFS Final Rule for CY 2021
Time to Set Things Straight
Now, let’s go back to our original questions: Does the AMA and CMS define total visit time differently? Do we use the total visit time or the average time? Novitas said it best:
“For dates of service on and after January 1, 2021, time is defined as the minimum time not the typical time and represents the total physician or qualified health care professional time on the date of service. The use of “date-of-service time” builds on the movement over the last several years by Medicare to better recognize the work involved in the non-face-to-face services, like care coordination. This definition applies only when code selection is based on time and not MDM. “
Both AMA and CMS have aligned on allowing O/OO E/M service being reported by either Medical Decision Making or Total Visit Time. Both have aligned on the definition for total time. And both have aligned on the time ranges used for calculating the O/OO E/M service level.
Total Time is defined as both face-to-face and non-face-to-face time personally spent by the physician and/or other qualified healthcare professional(s) on the day of the encounter. This does not include the time spent on activities normally performed by clinical staff. Below is a list of activities that may be counted toward a physician’s total time:
- Preparing to see the patient such as reviewing the patient’s medical record.
- Obtaining and/or reviewing separately obtained history
- Performing a medically appropriate history and examination
- Counseling and educating the patient, family, and/or caregiver.
- Ordering prescription medications, tests, or procedures
- Referring and communicating with other healthcare professionals when not separately reported during the visit.
- Documenting clinical information in the electronic or other health record Independently interpreting results when not separately reported.
- Communicating results to the patient, family and/or caregiver
- Coordinating the care of the patient when not separately reported
Leveling O/OO E/M on Time
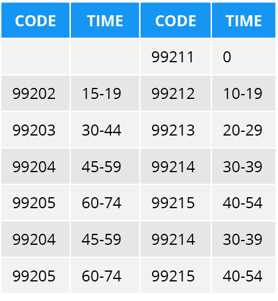
This alignment between the AMA and CMS is long overdue, though it is still far from perfect. AMA and CMS do not align on applying the same prolonged codes, nor time ranges to the O/OO E/M services. As a result of this difference of opinion, we are left with using 2 different Prolonged E/M codes and 2 different time ranges.
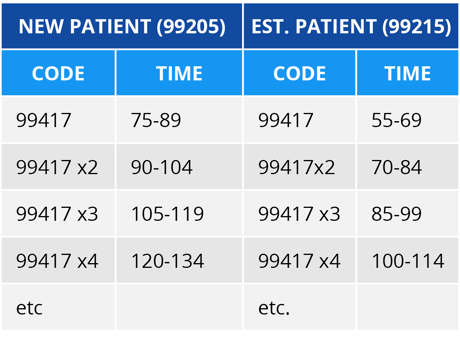
AMA instructs us to use code 99417 – Prolonged Service – when the office or other outpatient service has been elected, using time alone as the basis, and only after the total time of the highest-level service (i.e., total time of the highest-level service (i.e., 99205 or 99215). AMA defines use of 99417 by stating:
“Prolonged office or other outpatient E/M service(s) (beyond the total time of the primary procedure which has been selected using total time), requiring total time with or without direct patient contact beyond the usual service, on the date of the primary service; each 15 minutes (List separately in addition to codes 99205, 99215 for O/OO E/M services).”
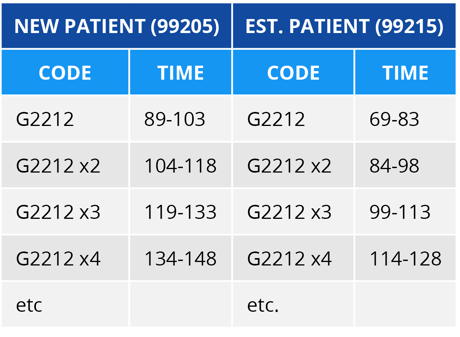
CMS notes they are not opposed to the concept of reporting Prolonged O/OO E/M services, they believe there should be a single prolonged code specific to O/OO E/M visits that encompasses all related time, and this time does not start until the maximum time has been met (see the CY 2020 PFS final rule for a more detailed discussion of this issue, (84 FR 62849 through 62850)).
CMS stated: “We believe there should be a single prolonged code specific to O/OO E/M visits that encompasses all related time. CPT®’s definitions of total time and usual time is confusing. We believe prolonged time can extend across date of service and be applied to any level EM service as long as prolonged time is greater than 15 minutes. To resolve the potential inconsistency of our policy with CPT® code 99417, we are creating a new HCPCS code G2212 to be used when billing Medicare for this service instead of CPT® code 99417, starting in 2021. HCPCS code G2212 is as follows:
“Prolonged office or other outpatient evaluation and management service(s) beyond the maximum required time of the primary procedure which has been selected using total time on the date of the primary service; each additional 15 minutes by the physician or qualified healthcare professional, with or without direct patient contact (List separately in addition to CPT® codes 99205, 99215 for office or other outpatient evaluation and management services)”
Notice the difference in the definitions? While each guideline speaks of 15-minute increments, the AMA lists “each 15 minutes” while CMS lists “each additional 15 minutes.” Basically, this means that AMA allows a prolonged service at the beginning of the first 15 minutes beyond the maximum time for the O/OO E/M Service. Whereas CMS does not allow a prolonged service until the full 15 minutes past the maximum time of the O/OO E/M Service has been met.
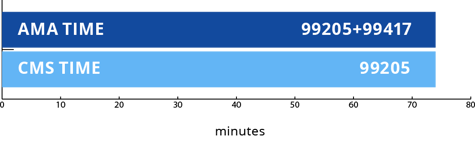
The key to understanding the different guidelines is to think in 15-minute increments. Imagine a ruler with etches for each minute of the day. When a provider begins their evaluation of a new patient, a deep etch is marked on the ruler to indicate their start time. Another deep etch is marked on the ruler at the end of the visit time, once the provider has completed their documentation in the patient’s medical record and looks at their schedule to see who their next patient is. Let’s say that the total visit time documented is 75 minutes. If we take a closer look at the ruler and see that for a New Patient, the provider’s total time exceeded the maximum of 74 minutes. Therefore, when applying the AMA guideline, we can report 99205 + 99417. However, for CMS we can only report 99205.
Total Visit Time: 74 minutes
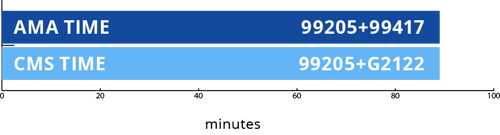
If the total visit time was 89 minutes, then we would be able to use the CMS Prolonged code G2122. The AMA calculation would not change because a second unit of 15 minutes is not yet met.
Total Visit Time: 89 minutes
Tips for Using Prolonged Codes:
- Codes are reported in 15-minute increments.
- Midpoint rule does not apply.
- Total time must fall exactly into the specific time ranges for the Prolonged code and/or units to apply.
- AMA allows Prolonged code (99417) to be applied at the beginning of the 15 minutes.
- CMS allows the Prolonged code (G2122) to be applied at the end of the 15 minutes.
- Do not report G2122 for any time unit less than 15 minutes.
- Do not report 99417 or G2122 in conjunction with 99354, 99355, 99358, 99359, 99415, 99416.
- Code G2122 should only be reported on Medicare claims, unless otherwise directed by the payer.
AMA Prolonged Time Calculations
CMS Prolonged Time Calculations
AMA also released revisions for the Prolonged Clinical Staff services (99415, 99416) with Physician or other Qualified Health Care Provider. These changes can be found in CPT® 2021 Professional Edition book, and not on in the AMA 2021 E/M Guidelines released in 2019. In previous years, these codes were based on time spent beyond the average time of a given E/M service. Because we are no longer using the average time for O and O/O services, it makes sense that these codes also needed to be revised.
CPT® now states:
“Prolonged clinical staff service (the service beyond the highest time in the rage of total time of the service) during an evaluation and management service in the office or outpatient setting, direct patient contact with physician supervision; first hour (List separately in addition to code for outpatient Evaluation and Management service.)”
What this now means, is that once the highest total time in the time range of the code description has been met, the prolonged clinical staff time can begin.
Another revision to code 99415 is that AMA changed the “less than” requirement from 45 minutes to 30 minutes. CPT® now states:
“Prolonged services of less than 30 minutes total duration on a given date is not separately reported.”
There are no changes for code 99416. We would still report this code for each additional 30 minutes beyond the first hour.
For example:
If a physician performed a 99213 evaluation which had a total visit time range of 20-29 minutes, and the clinical staff provided 42 minutes of prolonged face-to-face services, then the prolonged clinical staff time would begin after the 29 minutes. We could report 99415 x 1. If the clinical staff prolonged time was 120 minutes than we could report 99415 x 1 and 99416 x 1.
Tips for Using Prolonged Codes:
- Time must be face-to-face time.
- Total time must fall exactly into the specific time ranges for the Prolonged code to apply.
- Use with codes 99202-99205 and 99212-99215.
- Do not report codes 99354, 99355 with 99415 or 99416.
- Facilities should not report these codes.
The 2021 CPT® book includes an awesome Prolonged Services Comparison table, on page 45, that includes the above prolonged codes as well as a few others. I have mine flagged for a quick check when I’m auditing prolonged services, and I recommend doing the same.
Time is an essential component of coding Office/Other Outpatient E/M services. As coders and auditors, we can eliminate the confusion surrounding time-based coding by following these three easy steps:
- Understand the new 2021 Office/Other Outpatient E/M guidelines.
- Understand how and when to apply the rules.
- Work with your providers to ensure their documentation can stand up to the scrutiny of any payer.
In doing so, we can all ensure proper coding and payment of E/M services for our organizations.
To download this blog as a PDF, click the button below.


Questions or Comments?