My Report from the AMA CPT® and RBRVS Symposium, 2020

e/m coding, CMS, cpt, e/m services, ebrief, CPT codes, HCPCS, AMA CPT Symposium, outpatient services, Proposed Physician Fee Schedule Rules, e/m changes, RBRVS Symposium
I’ve been privileged to attend the annual AMA CPT® and RBRVS Symposium event nearly every year since 1998. Of course, as with so much in 2020, this year we did things a little differently. We did not gather in Chicago, like in years’ past, but instead connected virtually using technology. If we’ve learned nothing else this year, it’s that we are all becoming much more technically proficient - whether by desire or necessity.
The symposium, as always, was jam packed with information! New codes, deleted codes, rationale for changes and updates, RVU updates, and more. Also, unlike most years, the Physician Fee Schedule Final Rule had not been released prior to the symposium, leaving a great may questions unanswered.[1] Our new total CPT® codes for 2021 is 10,623, with a total of 329 changes, most of which (by my count) live within the Pathology/Lab and Appendix O - Proprietary Lab Assay and PLA sections. The runner up for the number of new changes is Category III codes. Category III codes are a temporary set of codes for emerging technologies, services, and procedures. Category III codes are not assigned an RVU value - but this does not mean they are not payable services. Payment rates for covered Category III services are determined by the payer. If you are providing services described by this code family, it is important that you use the correct Category III code, and do not select a Category I (5 digit) CPT® code that ‘almost’ fits.
A lower ‘COUNT’ of changes occurs in the Evaluation and Management (E/M) code category, though the impact of the changes to E/M services affects virtually all specialties.
We have the revised Office or Other Outpatient code changes that were described in the 2020 Final Rule ready for implementation in January 2021. Those changes remain as planned. As a reminder, 99202-99215 (99201 is deleted) will be described by the complexity of Medical Decision Making (MDM) or by total time on the date of service. As a result, us coders and auditors will need to learn a totally new approach to calculating the complexity of MDM. While we still have a three-element chart, from which two elements support the MDM level, these elements are significantly different.
For more tools and information on the 2021 E/M Changes, I recommend these two webinars and our free worksheet:
Everything You Should Know About the 2021 E/M Changes (Webinar)
2021 E/M Changes: Everything Else You Should Know (Webinar)
AAPC 2021 EM Interactive Specialty Webinars
There are notable updates to Chronic Care & Complex Chronic Care Management Services (1 new add-on code and 3 revised codes.) The new code, 99439, is an add-on to report additional clinical staff time during the month. It is important to note that you may only report a maximum of 2 units (40 additional minutes) and that the time in this code is a threshold, and the midpoint time rule does not apply. The revision to Complex Chronic Care Management includes changing “substantial revision to care plan” to “monitoring care plan.” This language aligns with Medicare’s guidance related to these codes.
Online Digital Evaluation Services (e-visits) 98970, 98971, 98972 language has been updated by replacing “Evaluation” with “Assessment” to match CMS’ G-code language for reporting e-visit services provided by individuals who may not report EM codes.
One of the most asked questions during this years’ meeting was related to CMS’ Proposed Rule, which outlines a different interpretation for reporting prolonged office services. The new code contained in the CPT book (99417) is defined as:
“Prolonged office or other outpatient evaluation and management service(s) beyond the minimum required time of the primary procedure which has been selected using total time, requiring total time with or without direct patient contact beyond the usual service, on the date of the primary service, each 15 minutes of total time (List separately in addition to codes 99205, 99215 for office or other outpatient Evaluation and Management services).[2]“
The definition is followed by an instruction to report with 99205 when 75 minutes of time are reached, and with 99215 at 55 minutes. The time threshold is calculated from the lower time of the time range in the new definitions. “99205 Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and high level of medical decision making. When using time for code selection, 60-74 minutes of total time is spent on the date of the encounter.[3]”
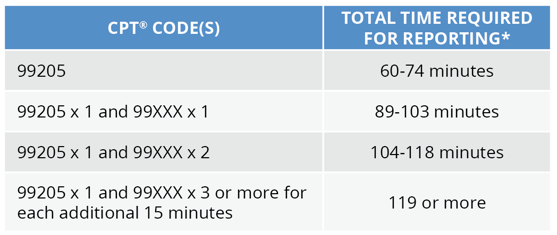
CMS, however, felt that the prolonged service should commence after the time range of the codes and published an alternate time schedule in the published Proposed Rule.[4]
Proposed Prolonged Office/Outpatient E/M Visit Reporting -
New Patient
*Total time is the sum of all time, including prolonged time, spent by the reporting practitioner on the date of the service of visit.
This difference in time created a slew of questions from those in attendance, all of which would go answered during the conference. When asked, the CMS representatives answered that we would have to wait for the Final Rule. CPT® panel members described the thought process that led them to the wording in the CPT® manual, which only left attendees still unsure if the two sets of time would be reconciled into one for implementation in 2021. Fortunately, the Final Rule was put “on display” December 1st, and we now know that CMS will not use the CPT® code, but rather they instruct providers to submit the new HCPCS II code, G2212 for prolonged office services are submitted for payment for Medicare beneficiaries.
In summary, attending this year’s conference was an altogether different experience, but with so many changes, and so much in flux, gathering information for the coming year remains at the top of my priority list. Even with the delay in releasing CMS’ final rule, the AMA and CMS representatives presented a comprehensive picture of new, revised, and deleted codes for the new year. We encourage each of you to read all the “green print” (i.e., updated or new guidelines) found in your print CPT® manual, review appendix B carefully to locate changes that will apply to your practice for additional study, and most of all, prepare for the changes to Office E/M services for 2021. To help you on your way, be sure to check out the resources available at the links we listed above.
Office services account for roughly 20% of Part B spending, and the change will impact virtually all specialties. If you have not yet prepared, or you would like some help, please reach out to Audit Services Group at 866-200-4157, or visit us at www.aapc.com/business.
To download this blog as a PDF, click the button below.
*CPT Copyright 2019 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association.
References:
- [1] Final Rule was released December 1, 2020 and I will include answers learned since the symposium.
- [2] 2021 CPT® Manual, Professional Edition, AMA Press, pg. 43
- [3] Ibid, pg. 19
- [4] Proposed Rule, Revisions to Payment Policies under the Medicare Physician Fee Schedule, Quality Payment Program and Other Revisions to Part B for CY 2021 Table 22, page 180. https://www.cms.gov/medicaremedicare-fee-service-paymentphysicianfeeschedpfs-federal-regulation-notices/cms-1734-p




Questions or Comments?