Episode 87:
Critical Care Anywhere: Exploring Tele-ICU's Impact
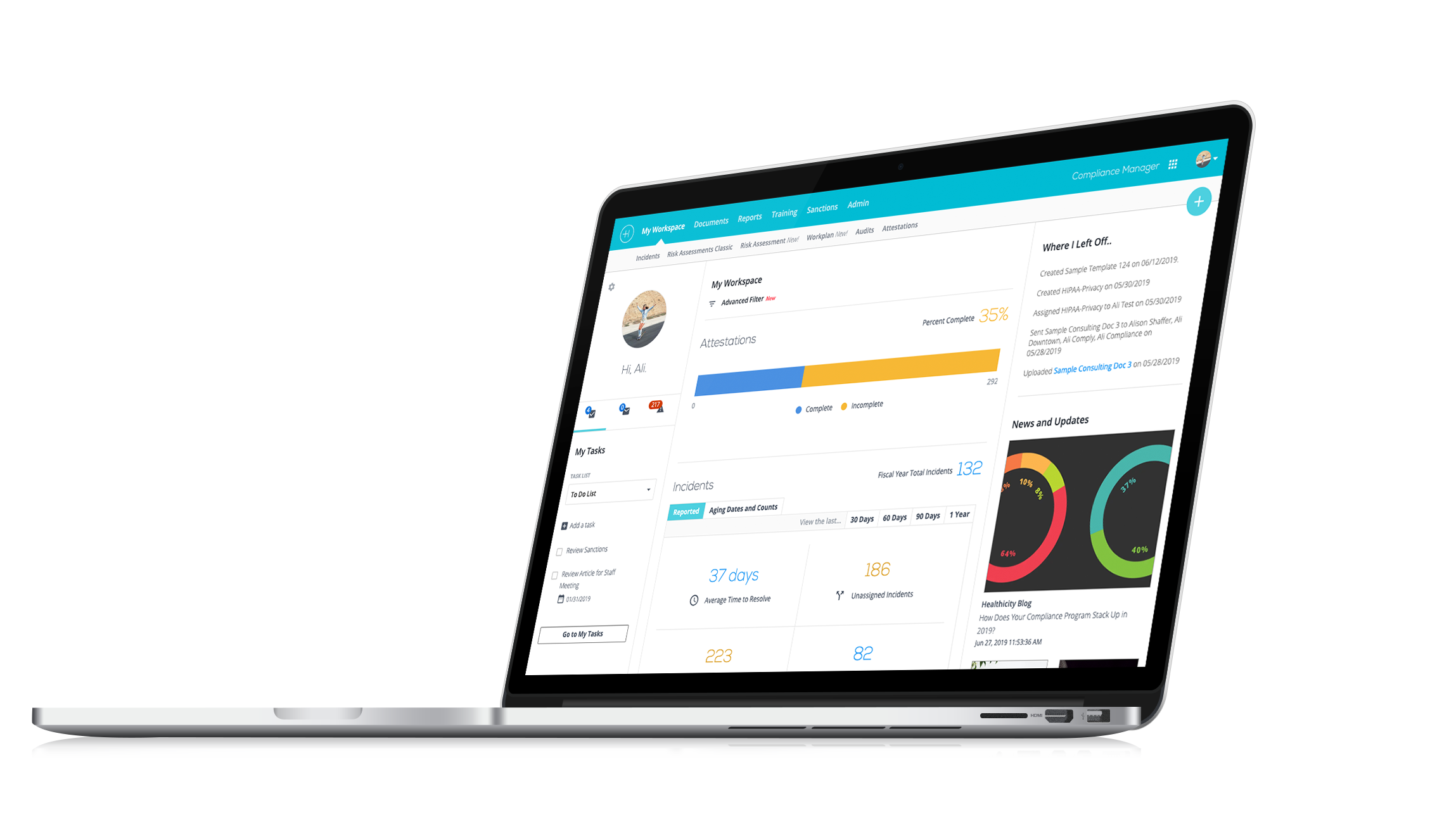
Watch the demo:
Compliance Manager
See the only all-in-one compliance solution today.
Discover how Tele-ICU is revolutionizing access to critical care in remote areas with expert Jeni Colarusso on the latest episode of Compliance Conversations.
We're thrilled to share the latest episode of Compliance Conversations featuring a Jeni Colarusso, a seasoned nurse and an expert in telehealth and Tele-ICU systems. In this episode, Jeni dives deep into the transformative power of telehealth, particularly in critical care environments.
Episode Highlights:
- Jeni’s extensive experience in surgical and cardiac ICU settings.
- An in-depth look at Tele-ICU and its role in expanding access to specialist care in remote areas.
- The impact of technology on patient outcomes and hospital efficiency.
- Insightful discussion on overcoming healthcare disparities through innovative telehealth solutions.
Jeni shares not only her professional journey but also gives us a peek into the future of healthcare where geography no longer limits access to top-notch medical expertise.
We hope you find this conversation as inspiring and informative as we did!
Interested in being a guest on the show? Email CJ directly here.
Episode Transcript
CJ: Welcome everybody to another episode of Compliance Conversations. My name is CJ Wolf with Healthicity, and today's guest is a dear friend but also an expert in her field, Jeni Colarusso. Welcome Jeni!
Jeni: Thanks, CJ! Good to be with you.
CJ: It's so good to have you on. I really appreciate your willingness to share your expertise, everybody Jeni is a wonderful nurse and have expertise in telehealth, as well as other things that will let her tell us a little bit about. But we're going to talk today about kind of telehealth, the advantages that it can have clinically and all sorts of good things. So, before we get into our great topic, Jeni, we'd love to have our guests just kind of share a little bit about themselves. Whatever you're comfortable sharing. If you'd like to tell us a little bit about, you know, your professional journey or anything.
Jeni: Okay, yes. So, I have been a nurse at one of the big hospitals here in town for 24 years. Pretty much all my time has been in critical care in the surgical ICU when it was a combined unit, when we got all the transplants, all the traumas, all the cardiac so it was an amazing place to practice nursing, I was there for 12 years and then I was on the ECMO team and did all the cardiac mechanical support and then traveled all over the Intermountain west, you know, go pick up patients and help care for them, inpatient, outpatient and in the OR. And then for the last, gosh, since 2016, I have been running one of the Tele-ICU programs for one of the, again, big hospitals here. So again, all my times been in critical care, I do a lot with educating the nurses in the Intermountain west who have our program, a lot of them don't have educators, so, I do teaching every week and again, just trying to work on again that critical care kind of component and then one fun fact I didn't tell you, CJ, when my husband and I lived overseas when I first took my nursing NCLEX and I realized we were going to be there for three years and I had to get nursing hours. So, if you ever watched the show MASH, you know, when they would send people to the 121st hospital in Seoul?
CJ: Yeah?
Jeni: That is actually an army hospital on an Army base. So, I volunteered in their ICU in their recovery room and for that, they let me take classes for free so I could get enough contact hours to renew my license the first time.
CJ: That is awesome. Now, I knew you guys were in in Korea for a while. I did not know you were doing that all these years. I've known you well, that's cool.
Jeni: I know. Yeah, fun fact.
CJ: Yeah, well, thanks for sharing that. And Jeni, you know, we have a lot of like healthcare folks as our audience mostly compliance and regulatory folks, but some of them are clinical but some aren't and I just wanted for their benefit you mentioned ECMO and then I know you talked about the VAD tell us what ECMO is and what a VAD is?
Jeni: Oh yeah, think so. ECMO is a short term like heart lung bypass. So, you can put somebody in the OR or in the ER in operating room or the emergency room and it just helps their either lungs or heart or both rest depending on how it's set up. And then a VAD is a Ventricular Assist Device so it's an implanted device. I don't know if you guys remember Vice President Cheney had one, so it's when somebody has their heart is failing and they need assistance, and sometimes they have it for the rest of their life, and sometimes they have it until they can get a transplant.
CJ: Yeah, exactly. So, Jeni has, you know, all this experience in in surgical ICU and then I knew you had all these years in kind of the cardiac space where just like you said, people who might have failing ventricle or failing heart, they need a little bit of push and yeah, keep going.
Jeni: exactly!
CJ: That maybe that's a whole other topic. I'll have to talk to you about because technology has probably just like gone way beyond me, but that's cool stuff. But we wanted to talk about ICU and so tell us when we hear Tele-ICU like, what should we think because you know all of us live through COVID, right? And before COVID now know telehealth didn't really get over that hurdle, of course it existed in all forms and fashions, but it seems like it really pushed us over. I know your involvement as well before COVID, but a lot of us that aren't, you know, clinical might think; "Oh telehealth! Yeah, I got the sniffles. I'm going to call my doctor and going to see each other on camera. He's going to prescribe something and all is great. I didn't have to go into the office," and that is an important part of telehealth. But tell us a little bit more about like this Tele-ICU.
Jeni: Yeah! So Tele-ICU is a way to bring expertise of and for this example intensivists to smaller hospitals and some that are not so small. So not everybody is going to have an intensivist to run their ICU. So, it brings that intensivist essentially, you know, a phone call away and can go on camera just the same way you would call like the example you gave about the cold, the providers and these other hospitals can call and speak, you know to our providers and get that consultation. With the big goal of trying to keep people in their home communities as long as it's obviously appropriate, but as long as possible.
CJ: Yeah, it's such an awesome concept and I benefited from it personally years ago, actually during COVID I was having a surgery unrelated to COVID or anything, and I had some complications. I ended up in an ICU, but my surgery was, you know, at a local hospital. So, you know, I'm here in the Salt Lake area. I was not at, you know, the big, you know, the big flagship hospitals with all the experts. But I didn't have to be transferred. So, they consulted with these experts because that local hospital was a good hospital and had all the right people, they just need a little expertise to get me over that hump. And so that's kind of what we're talking about, right?
Jeni: Exactly! It's such a great resource again, just to help again, just the idea of two heads are better than one, and you know a lot of the smaller hospitals, even local hospitals they have, you know, their providers there, they don't have people just swarming around like you said like some of the bigger hospitals with all those sub specialists. So and they don't need them all the time so having this really spreads out the love.
CJ: Yeah, such a great way to do it. And you know, as we were communicating beforehand, I could sense your passion for it because you're like. You know, well, maybe you can kind of put some color on this, but like, why should people have to? Like, why would the patient have to get on the helicopter, fly one way and all the family drive, you know, 8 hours, 6 hours to that hospital when a lot of this can just be done locally and without this disruption, right?
Jeni: Oh yeah, absolutely! With your VAD patients, everybody was displaced. Everybody had to come to the Salt Lake area. And that's hard. You know, you don't have your support system. You don't have your loved ones, as you mentioned, when you fly to, you know the Salt Lake area, it's a one-way trip and a lot of people don't know that. And a lot of people live really far away. So, whether their loved ones are driving or having to take off work to come, you know, visit and then they're trying to figure out where to stay and what to eat and they're still dealing with the stress of, you know, their loved one being in the hospital as much as possible, keeping people in their home community. We know, you know, there's a lot of research on it showing that people heal better with their families around them, it helps with even like delirium and just all kinds of healthcare issues not to mention just their comfort and keeping those healthcare dollars in those small hospitals. We have a lot of small hospitals closing and in these rural areas and then maybe the last point I want to make is I just don't think personally that where you live should determine what kind of healthcare you can get. I mean, telehealth is the way, the only way truly that we are going to have healthcare in every you know, nook and cranny of our very big country.
CJ: Yeah! And that's kind of the sentence when we were communicating that I loved hearing from you is that it's like everyone deserves that, right? And the way to get this is, you know, telehealth as a way to get it, right? So, I just, I love that so thank you for sharing that and thank you for being passionate about it and I could sense and view the kind of the focus that you have is really, let's use the limited dollars we have the best way and best outcomes. You mentioned research about you know patients just do better in their own place, right? And family and stuff and that can be scientifically quantified it sounds.
Jeni: Yeah, it can. It absolutely is. And it's again. So, it's really, it's really important and we've been lucky with a lot of the things continuing, you know the funding with telemedicine through COVID like you said, it really shined a light on all that we can do. And you know previously ZOOM meetings were like what? And now everybody you know knows what they are it's a lot more familiar to people, so yeah, it's we've been very lucky to have the, you know, continued support and such.
CJ: Yeah! So, one thing I wanted to ask you and you kind of mentioned it kind of the different models of telehealth like a consultative or if I said that right or a bunker model, tell us a little bit about different models and how they work and benefits, pros and cons of different models.
Jeni: Yeah! So, there's a bunker model where essentially you know each bed of a remote hospital will be wired and then that information is streamed kind of to a central hub. Some people have proprietary software where they can, you know, one nurse can watch 50 people on the screen per se and they are just kind of watching like circles green, yellow, red. Because as a nurse I can't watch, you know, more than 3-4 or five patients well, and remember everything about them, you know, but with technology then you can help, you know, other hospitals watch more patient. So though that information kind of streams through and then if there are issues, then the person the nurse, you know watching, can you know, call into the room to speak with to the nurse or they're available for questions or they could be, you know, another person to like document for example, if there was a code blue or something like that where you kind of need more hands. And then the provider is there as well. Sometimes they'll do orders and stuff like that. It's expensive, though, because you've got to wire all the beds. You know, you've got to have 24/7 on call of multiple people and obviously backups.
A consultative model, is more like call us when you need us. Some of the smaller hospitals don't have patients in their ICUs all the time, so to pay to wire beds and stream that is, you know, maybe not as cost efficient for them. Some people, it doesn't make sense. Some people it doesn't. So those are kind of two different models of using Tele-ICU.
CJ: Awesome! That is really, really interesting. We're going to take a really quick break and we're going to be right back and talk some more with Jeni.
Welcome back everyone from the break. My guest today is Jeni Colarusso, expert and friend. I got to keep putting that friend in there because lots of people that I like, but I've known you so long you're a great person and a great nurse. And we're talking about ICU, Tele-ICU, those sorts of things. Jeni, I wanted to ask you. I know you're the clinical expert in all of this. A lot of our audience deals, you know, kind of with rules and regulations. I'm curious if you ever get involved and if it's just a yes or no, that's fine, but or you know, if you have more to share, like what kinds of barriers are there like with regulations, you know, you know, we talk about HIPAA a lot, and I don't know if you get that involved or, you know, what kind of training the clinicians get and you know, is this a secure system? Is the data secure, you know, coding, billing. Does any of that ever come up in your line of work or does? Somebody else, kind of take care of it.
Jeni: No, it absolutely does. Of course, HIPAA, yeah. So, we have to make sure that everything that we do is HIPAA compliant. So, we try to make the information that we're sending back and forth, obviously secure HIPAA compliant, but using equipment and systems that are the least expensive for the facilities as possible, we work with some really small facilities and a lot of what we can do, we just use iPads. And then the software is HIPAA compliant, so it's great because you know an iPad doesn't cost a whole lot or they can use whatever tablet they want, you know. And if you have to replace that every three or five years, that's not a very expensive proposition. The other thing that you mentioned with compliance and all of those kind of thing is licensing, it's hard because you have to have licenses in all the states where your providers work. The compact really helped with that a lot because it made it for providers to be able to get multiple licenses in multiple states, but you still have to do individual DEAs if your providers are prescribing and that's very expensive.
CJ: Interesting!
Jeni: Yeah! And then you know different, again, different states have different regulations and different requirements for continuing education and you know, registering for board of, you know, their pharmacy boards. You know, there's a lot, there's a lot that goes into it.
CJ: Yeah, that was going to be one of my questions so I'm glad you kind of brought up. It's kind of like multi state because you know if you're in an area like we are where there's a lot of rural areas in neighboring states, too, and you know large city might have the best XY or Z and so you're talking about licensing and the compact. And so as much as you know, it seemed like nursing was ahead of the curve on this, like nurses compact, you know, where licensure applied across state lines and but tell me if that's true, and then also our physician licensing compacts like that exist, tell us what you know.
Jeni: So, nursing compact has been in place for several years, many, many years. I can't tell you when, but yeah, it's been many years and then physician compact that is new, it happened probably like three, I want to say three years ago. So that's been huge for telemedicine. It makes it much easier because again previously you had to apply to every single state and get approval for every single state and going through their boards and it was very time intensive, very labor intensive this with the compact, I don't want to say it's easy, but it's definitely easier because it's one and you know one and done. So, you know having them catch up has been extremely helpful for telemedicine.
CJ: Yeah, and my suspicion, I'm curious what you think is, you know, telemedicine is, I mean it's just it's going to get bigger and bigger my suspicion is that these roadblocks and barriers and regulations, though they're important to some degree, are going to maybe become more consolidated and easier. Are you seeing any of that in the near future or is that more still hopeful like longer term?
Jeni: No, I definitely think that there are, I think again, like you said, COVID shined a light on how, you know, healthcare disparity that exists just because of, you know, regional where you live and just the sheer number of providers like you know I can't quote you the statistics you know off the top of my head but it's, you know, we only have X number of neurologists, so every little town is not going to have a neurologist but could they really, you know, use one need one at times? Yeah, for sure. But could a small hospital afford to keep one on staff all the time? No. So, that's a way to kind of overcome that. So, I think people I think again COVID, you know, you don't want to waste a say you don't want to waste a pandemic or crisis kind of thing. Let's take away the good parts of it what we learned and how Telemedicine can play a really important role in providing that. So, I think a lot of the emergency approvals, those were extended for several iterations and then it's given, you know, legislatures time to kind of catch up and again like the physician compact that exists now again I think it's helping those kinds of things to catch up. But I think it's given people just that vision of what's possible.
CJ: Yeah, you know you mentioned neurology, so you kind of brought up specialty. So, tell me like with Tele-ICU, are they like, are the physicians and the nurses, are they trained mainly as intensivists? Or do you integrate others like maybe you might have a neurosurgeon, I know surgery might not be done over the phone, of course, but you have neurosurgery consults, your neurology, do you have cardiology? Like who are the specialists in, like a Tele-ICU program?
Jeni: So, the initial call are just intensivists, but then it's like, you know, for example, nobody's going to know everything. I mean, it's just not possible. So, if my provider doesn't, you know, doesn't know it's out of their wheelhouse or whatever, you know what they're going to go call the ID attending and that's sort of the, you know the beautiful part about ours is you're calling and speaking to an attending as opposed to you know kind of having to work up from the lower echelon, you know, resident students wherever given you know where you are, it goes right into an attending. And if my attending doesn't know it well, then they're going to call the, you know, ID attending or the burn attending or whatever other attending to get the answer. So yeah, you tag into the whole system and it's a quick way to do that. You know, TeleBurn has been around for, gosh, almost 25 plus years. Telestroke like 20 years. So, there are more and more specialties, you know, Telederm, I mean, there are so many because again, just that value of having specialist again, we're just getting, we have fewer and fewer doctors. So, we're, you know, nurse practitioners have been great. But again, they're limited in number, so spreading it around is kind of the only option we have.
CJ: Yeah, it's kind of exciting and for selfish reasons because I don't know if I can ever convince my wife of this but one day I want to live more rural and it's like, as long as they're in the hospital, they can connect to some expert academic medical center or something where I would get help if I need it then maybe I can get there.
Jeni: Yeah, no, it makes it again, it makes, I mean, I leave the Salt Lake valley and I'm like; "What hospital would I go to?" Yeah, that's my, you know, we saw traumas for a long time, so I'm still scarred by that and but it makes a big difference, like, if I know somebody has a telemedicine program with another big facility, again, I personally would be like, yeah, that's where I want to go because if they kind of again get a little bit out of their comfort, then they've got somebody else to talk to and academic medicine is great because you collaborate, right? Well, let's get that to our other facilities so they can collaborate as well. There's, you know, it really needs to, you know, kind of be more across the board.
CJ: Exactly! So, on this consultative model is it basically phone calls and then that maybe sharing the images X-rays, lab results, EKG tracings, whatever the diagnostic, you know result may be is that basically kind of what this is?
Jeni: Yeah! So, it starts out with a phone call and then if you know, if needed, they can go on camera at any time. Sometimes you know patients want to go to the big medical center because they think they somehow have a different answer, yeah! When it's like, no, we've done, you know everything they can. We actually had a call like that where a patient was going to pass but the family wanted to know that they were had done everything that they could which, you know, I totally appreciate. But they called Tele-ICU, they spoke to our provider who also happen to be a trauma surgeon. And he's like; "You guys have done everything I'm going to. You know, you're welcome to transfer him, but again we there, you know, then everybody could stay there and say goodbye and they didn't spend, you know, $18,000 flying the patient one way to you know to Salt Lake, so it really, you know, it's a better kind of way.
CJ: Let me ask you something too, as we're getting kind of closer to the end here and you may or may not, this may or may not may not be your wheelhouse and that's fine if it's not but because you're in kind of this expertise of telehealth even though you know specific to Tele-ICU, you may run in the same circles as other conferences, and you're hearing the latest on other telemedicine techniques, like, you know, robotic surgery from a distance or you know, like I know radiologists who read images from another state or pathology, who now they're digitizing, you know, pathologic slides and just getting good enough that that they feel like I can make a diagnosis from the screen. Are you aware of other telehealth progress and those types of things?
Jeni: Yeah, let me think about that. I mean, I know most of our other facilities use like a Tele-pharmacy type program because again they'll have pharmacists during the day but not on call at night because they just don't need them that much.
CJ: Right?
Jeni: You know that occurs like you said, with radiology for sure that happens. Radiology was, I think one of the one of the first ones because again, you know when I need a thing, I mean, radiology is not sitting on the units anyway. That's always kind of the remote thing. So yeah, and I'm sorry I don't think I answered the 1st question fully I got on a roll and I forgot, but maybe they can go on camera, yes, but then yes, they can send images, they can review images you know, sent through software systems and that kind of stuff, so that is available to them, EMR integration is challenging because every site has their own EMR so we tried that for a while, but keeping ten providers up to date with, you know, 15 different EMRs and their logins at current was just too much so we scrapped that. But yeah, they do share their information we'll go back to that.
CJ: That's cool and I, and I'm just hopeful, you know, as technology advances. It's like, you know, maybe in my lifetime maybe it's already happened and I'm just ignorant of it. But like these remote procedures, right?
Jeni: Oh yeah!
CJ: Like if you get good enough systems with robotics and, you know, you could maybe get the best skilled surgeon or procedure list in one geographic location and because of the systems you're able to help that person obviously a lot more risks and things, complications that could happen, but that I don't know. Is that Jetson, you know, is that too futuristic that's not going to happen?
Jeni: No, I think it will. I think it will. Yeah, I think it will. You can have a surgeon there and you can have an expert surgeon, you know doing robotics. And I think you can bring that expertise. I absolutely think that's not that far away.
CJ: Yeah, cool.
Jeni: Yeah, I totally agree with you.
CJ: Well, Jeni, this has been awesome. I want to give you last word. If there's any parting thoughts any soapbox you want to get on or, you know, if you could change minds or if you were queen for a day, you know any or any last-minute thoughts. We just really appreciate your expertise and your willingness to share what you know.
Jeni: Yeah, I think probably my biggest soapbox is, again, just that what you had mentioned regarding getting barriers down so that way we can minimize healthcare disparity just with geographic location and numbers of providers, right? So, using telemedicine to the full extent of what it's you know capable of doing I think is just brilliant. It's a way to save healthcare dollars. It's a way to, you know, manage populations better. I just think there's so many bonuses and so many upsides to it. I just don't really see a downside.
CJ: Yeah, exactly! I kind of feel the same way, it's like and so it's exciting to me. So I was, I'm just really grateful that that you had some time to share with us.
Jeni: Yes!
CJ: Well, thank you, Jeni, and thank you to all of our listeners for listening to another episode. As usual, you know, if you have ideas of topics or speakers that you know, please share with us, we'd, we'd love to bring you discussions that are meaningful to you if you like this type of podcast, share it with your friends and subscribe. And until next time, be safe, everyone. Thanks for listening!