Episode 91:
Expert Tips on Gastrointestinal Coding and Billing
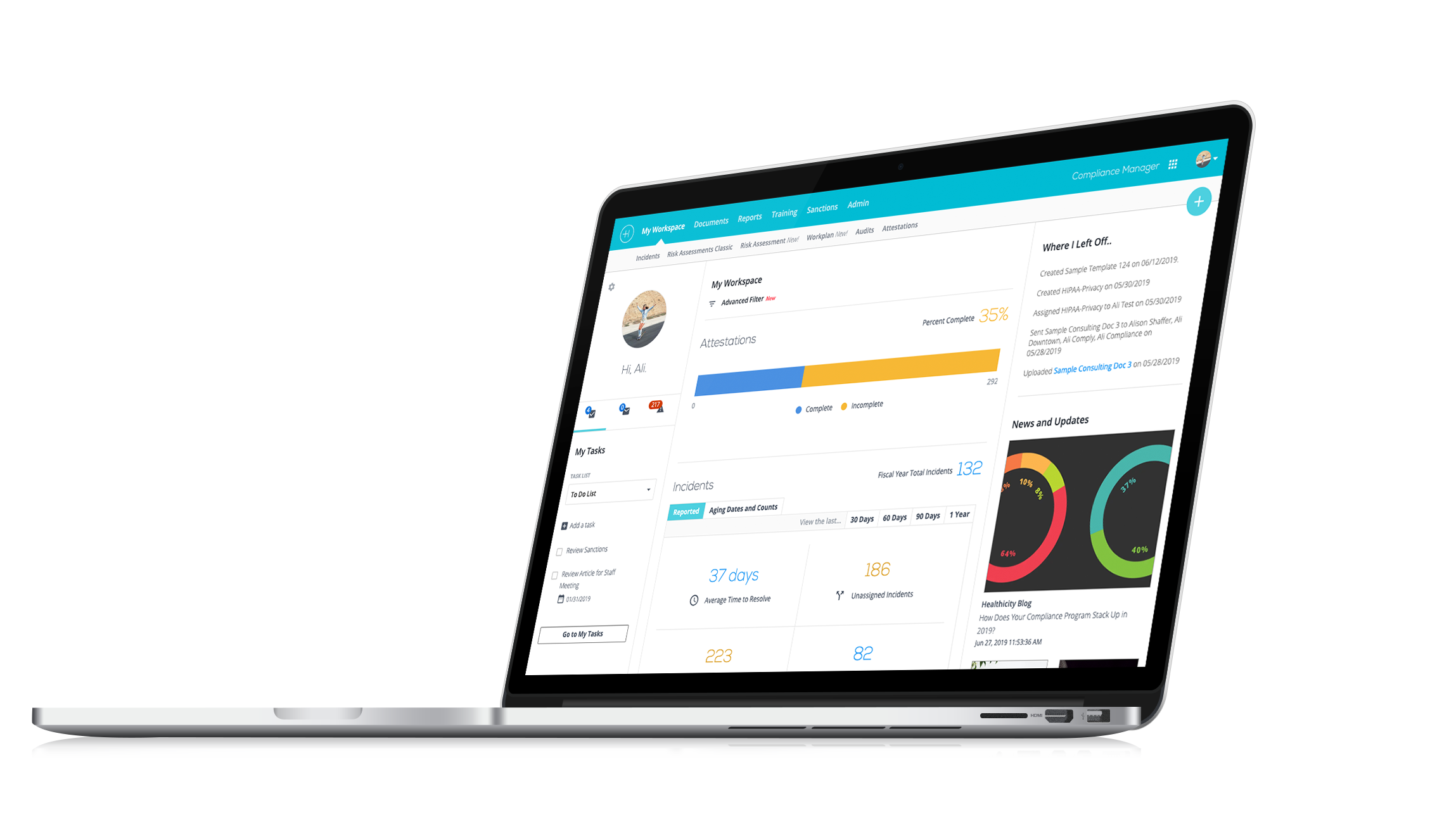
Watch the demo:
Compliance Manager
See the only all-in-one compliance solution today.
Discover expert tips on GI procedure coding and compliance in this episode of Compliance Conversations!
In this episode, our host CJ Wolf sits down with Laidy Diana Martinez, a coding supervisor, to discuss the world of GI coding and compliance.
Episode Highlights:
- Introduction to GI Coding Challenges: Understand the common hurdles and how to overcome them.
- Screening vs. Diagnostic Colonoscopies: Learn the critical differences and their coding implications.
- Essential Modifiers: Find out which modifiers to use and when.
- Documentation Best Practices: Discover what’s needed for accurate and compliant GI procedure billing.
- Medicare and Payer Policies: Stay up to date with the latest changes and requirements.
Laidy Diana Martinez, with her extensive experience as a coding supervisor, brings valuable insights and practical advice that can help enhance your coding accuracy and compliance efforts.
Interested in being a guest on the show? Email CJ directly here.
Episode Transcript
CJ: Welcome everybody to another episode of Compliance Conversations. I am CJ Wolf with Healthicity and we have a wonderful guest today. As always, we have wonderful guests. Welcome to the show, Laidy Diana Martinez.
Laidy Diana: Hi, CJ, how are you today?
CJ: Doing great. Thank you so much for taking some of your time to share with us some of your coding and compliance expertise and we'll get to that topic in a moment, Laidy, but we would love and we always love our guests to take a moment to introduce themselves, tell us how you got to where you are, what you're doing, you know, what you love about coding compliance, whatever you like to share a little bit about your professional story.
Laidy Diana: Sure, like I would love to do that. First and foremost, thank you for inviting me to be at your podcast. I'm honored to participate and be here with you guys. Well, like you say, my name is Laidy Diana Martinez. I'm an immigrant. I came from Mexico a few years ago. I've been on the health care for 14 years already. Wow, that's a lot, right? And then I'm currently, being a coding supervisor, I hope, but before I did this before I got this new role, I work in primary care and I learned all aspects of revenue cycle. So, I can say that I obtain all my foundations and that practice. So, I was very privileged that this provider gave me the opportunity to learn all the things that I know now, right? So, I'm currently like I mentioned, I'm currently the coding supervisor and the whole health systems here in California, it's a huge organization that I'm very happy to be in this place because I can able to contribute and help my fellow coders and coworkers when they have any questions or anything like that, so I'm very happy to be in this organization and like one thing that I love the most about coding it is helping others. I think that's one of my biggest passion and so anytime that I can able to contribute to someone's success, I'm the biggest cheerleader for someone.
CJ: That is so great and I have to tell everybody, Laidy and I met in person at the Healthcon conference, and she's just very friendly and very outgoing taking pictures. And I just wanted to tell you how much I appreciate your personality and how friendly you are, I think it's wonderful.
Laidy Diana: I think if I can describe myself other than being a coder, I can say that I'm motivator like I'm the hugest motivator. I mean, I feel like sometimes the world needs more people to put a positivity and then I think that when you give someone a positive thought you get kind of that domino effect, but in a good way, right?
CJ: Yeah, absolutely! It's like you're spreading the happiness and that can be contagious and you know, what we do sometimes we're telling people no a lot or you can't code that way or you have to document this way, and that can sometimes be a little bit of a downer. But having, I love your idea, your personality of just being positive and a cheerleader. That's a great way to put it so thank you for being that way.
Laidy Diana: Yeah, and I think just to really say something about that, I think sometimes when it comes to coding, when you don't take anything in the negative way, it kind of really helps you because there are going to be times that you're going to be criticized or not criticizing constructive criticism, right? But you have to be open to receive that feedback. Sometimes that feedback will help you to grow and make you a better coder. So, that's what I do with my coders, you know, and every time I'm going to address something, an error, technically they're not errors, they're opportunities to learn something that you can get out of it. So, I always encourage take the feedback because that feedback is going to help you in the long run.
CJ: Yeah! And I teach some classes for APC and some other things that I'm doing and I'm always telling students like; "I've been in healthcare for over 25 years. I'm still looking things up and still learning and it's just we need to have kind of that lifelong learning attitude."
Laidy Diana: Exactly!
CJ: And so yeah, the podcast and our topic today will help us all along in that lifelong learning, we're going to talk about gastrointestinal procedures and coding, Laidy has a lot of expertise in this area, but let's start first with just kind of a general question, you know, in your experience, what are some of the typical coding challenges in GI procedures?
Laidy Diana: Okay, so some of the typical challenges that I have faced and I constantly see in my current job I see the problems with specificity of diagnosis, you know, we had to always kind of make sure that we capture the specific that, you know, to the specificity and sometimes even those see codes or screening codes that we need to move. It's like the indication for the surgery. I have a friend that you probably know her, Christine Hall, and she always says; "What was done today? What was that today?" It's very specific. And then that's the number one thing I see that screening versus a therapeutic or multiple procedures and when to apply the proper modifier. And then, you know, but I think the biggest challenge is updating the policies and like making sure you're up to date because what happened today might not be able to be effective for in a later time. Like, you know, they just recently there were changes that happened last year on 2023 with GI with colonoscopies and what is considered complete colonoscopy screening and then so just keeping yourself up to date I think that's the biggest challenge.
CJ: Yeah, I totally agree. And GI procedures are so common, right? Colon cancer and some of the gastrointestinal cancers are some of the more common cancers that people suffer from. And so we're going to see, if you're a coder just starting, you're going to see a lot of GI procedures because they're very common.
Now, Laidy, you mentioned, you kind of briefly mentioned just screening and diagnostic, let's talk about that a little bit more. So, colonoscopies, we know our scopes, they insert the scope through the rectum going through retrograde, if you will, through the colon and they can do that for screening, right? Like when we all hit a certain age, there's recommendations that you should have a screening colonoscopy, even if you don't have any signs or symptoms. But then there's also diagnostic. Tell us a little bit about what you know about the differences between those two and how coding, why it might be important for coding purposes?
Laidy Diana: Well, it's correct exactly. And it all goes back to the payer. So, if we're talking about Medicare, they're two categories and the screening colonoscopies, right? So, we have the high risk versus non-risk. So it's so important to understand that not, you know, your NCDs and then read those manuals. You know, reading the NCD manual and making sure what's complying with the with the high risk or non-risk because that's going to determine how you're going to perform if the doctor and not pursuing a colonoscopy. If this is a high risk and it and he needs to meet all that criteria for high risk, that means that either still screening but you have to have a family history or personal history or specific conditions that fall into the high risk category. Then, if there's no symptoms, then it also just falls into the average risk, which is our G 0121 that normally does patients that they get, they don't have any symptoms and they cannot use that code. But yeah. And then then you have your diagnostic screenings, right? So that's when the patients have already a symptom and they or has already suggested like a history, but then again, I'm going back to the screening because I had this question and a lot of coders asked me this. So, if a patient comes in with a follow up our lesser billing colonoscopy, which is kind of like they follow up two or three or five years, right? So, is that considered still screening? And I said well yeah, the history might give you the high risk reason, right? So, the indication is a high risk, but it's still a screening. So, you have to code it as a screening. Now if it turns into diagnostic, that's a different story because you don't know what you're going to. The doctor doesn't know what he's going to find when he does the procedure until he performs it. So, once it's performed, and if that is a complex. This totally different story. Now it turns into diagnostic and there are proper modifiers depending on the payer that you must utilize.
CJ: Yeah, and that's a good point is that even though somebody's high-risk if they're having no signs and symptoms, it's still screening. They're just at a higher risk because of, as you mentioned, you know, they might have personal history or family history, but if they if they're not having signs or symptoms, that's really when something is screening.
Laidy Diana: Exactly!
CJ: Yeah! And I also, you know, you mentioned Medicare and making sure you're following either NCDs or LCDs and I think we're even seeing a lot of these procedures in patients younger than Medicare age and so on different payer cause I'm glad you mentioned, you know, being aware of what the payers policies are because if I remember right, the United States recommendations for screening is in your 40s, your first screening colonoscopy, I believe it used to be 50 and I think it might now be 45 or something.
Laidy Diana: Correct! That was changed last year. They made the call to change it from 50 to 45 and Medicare follows that guideline too. So, I think the majority of the payers are already following that task for recommendation to do it instead of 50 to 45.
CJ: Yeah! And so, it's important, you know, and a lot at age 45, there's going to be a lot of people who might not be on Medicare. So, you got to follow those payer policies they might only pay for one screening colonoscopy every so often. And so that's really important. Well, that's a really good, good discussion on screening and diagnostic.
Laidy, we're going to take a quick break here and then we'll come right back and talk some more about GI procedures.
Laidy Diana: Thank you!
CJ: Welcome back everybody from our break, we're talking to Laidy Diana Martinez and she has expertise in GI procedure coding and we've been talking about colonoscopies, let's shift gears a little bit, Laidy, and tell me what you know about documentation requirements for GI billing compliance.
Laidy Diana: Sure, there's a specific documentation that it requires, so the doctor really has to document when a procedure has been performed. They have to indicate the necessity for that procedure, the findings and any intervention perform performed. They also had to have consent form, right? So you also had to make sure that you're explaining to the patient what the procedures, the risk and you know all the specifics about the procedure that they're going to have, pathology reports, I think it's one is so important to know because sometimes as a coder, if there was a pathology performance, there was a biopsy, you had to kind of wait and this is something that it's a tip for the coders that you have to wait until you get the results from the pathology because you can code from the pathology report, because that can change the diagnosis that they say, for example, they remove a polyp and then that polyp was ended for biopsy. So you had to really wait to see what was the findings of the report, right? So, and that might change, maybe the patient just came in for or they removed a polyp and the polyp was a polyp removal. But then you don't know if that polyp was benign. So, you really kind of have to wait and then correct coding. Accurate and specific codes that might be used. Again, going back to the pathology. So, you have to kind of really wait and then if you're up to date with your coding, so it's maybe we'll consider like I always tell my coders just wait, maybe take one or two days, but at least you're going to make sure that even if it doesn't change, but at least you know that that is there.
CJ: And you know that's from a clinical standpoint, that's the whole point of these colonoscopies is if you're doing biopsies, it's finding out exactly what the behavior of that tissue is, is it benign? Is it a polyp? Is it, you know, precancerous, is it, you know, carcinoma in-situ or you know whatever it might be. So I think that's a really great point about waiting to make sure you look at the pathology documentation. So with a lot of colonoscopies and other GI procedures, you might need to use modifiers, right? Tell me a little bit about the different scenarios that modifiers might apply to in GI procedures.
Laidy Diana: So, modifiers like, yeah, that's the favorite topic for a coder, right?
CJ: Right!
Laidy Diana: So, modifiers, of course. You're going to see a few ones. I think there are a few that they utilize more in GI. I see in a lot of 59, 51, PT and 33, and I think 53 and 52, but depending on what was performed and that documentation let's say for example a provider perform a colonoscopy and it was a screening, but then he ended up removing a polyp by a snare technique which is our 45385. So now that is screening colonoscopy is no longer screening, it turned into diagnostic because the polyp removal, right? So, you have to, even though I still screen it was a screening because that was the indication you have to make sure you have your first listed diagnosis as the screening and then the polyp removal as your secondary and then adding modifier depending on the payer again because if it is Medicare you have to use PT modifier to indicate that this procedure turn it into diagnostic and then that deductible and the co-insurance is waived. Otherwise, it will not be denying if you don't use the PT modifier, because then you're telling that you're performing a procedure diagnostic that you're using your screening codes, diagnosis codes.
So, you have to be kind of very careful and then read those. Like again, I'm going to go back to Medicare and I think the NCD manual and the American claim processing manual could be your best two friends to always look, I always tell everybody those are your go to manuals that you're going to utilize the most is your NCD and your claim processing manual, because it has all that information that you need for all different type of settings and different type of specialties, right?
So yes, that's your PT modifier and now if it is a commercial payer, then you would use 33 which is the alternative for PT modifier, but for some of the payers don't recognize PT so then you will have to use alternative which is 33. If a procedure was discontinued due to poor preparation and then the provider wants to redo the colonoscopy, then you have to apply modifier 53, because this colonoscopy that you're performing right now, you could redo it, but then it will be payable at a lower price but a lower reimbursement, but you will still be able to get another procedure on a later time and then the frequency will not apply.
CJ: And that's a really important point because you know, even though patients do their best to prepare, we all have probably, if you've had a colonoscopy, you know, you drink a certain solution and you clean yourself out a little bit. But if that doesn't work completely and they can't do the full colonoscopy, maybe they only can do part of it or maybe they can't do any of it. That's a really hard because you have to, like you said reschedule to be able to...
Laidy Diana: Yes! And then then you. Of course, then we have a modifier are infamous modifier 59 which you can able to utilize when you perform diagnostic procedures. But you have to be kind of really, the documentation must support a distinct deletion or a different technique performed in a different anatomical colon area, so I think that is important too, that making sure that you read through the documentation and making sure that it supports. If two different techniques and two different missions were performed and remove then totally fine to code it, but it has to support it.
CJ: Yeah, and that's a great point and you know there may be multiple lesions throughout the colon you might have and you might do a biopsy and in the descending colon, but maybe you can do, you know, a destruction of a lesion or some other technique as you mentioned, maybe that's in the transverse colon. So you really reading that documentation. And then also you know, making sure that the physician understands as they dictate to make sure that the note is clear to show that these are separate locations or they're separate therapeutic procedures like you said, you might do destruction or removal in different ways depending...
Laidy Diana: Yeah! And I think you make a good point about it. Like when it comes to that, that's what I always tell the coders, if you see something is not clearly stated tell the provider before the claim goes out, because once it goes out, it is kind of hard because you can't, you know, reprocess the claim or re like having to admit that the documentation because it's already went out the door. So that claim has already like gone out. So but I do use those examples as a provider education, you know, so that way I can educate the providers, I can tell them you know what? This could be changed, but if you perform, if your documentation supports these codes, it probably happened. It probably did happen. I'm not saying that it didn't, but it's not being documented and you know our golden rule is always says; "It's not documented, it didn't happen."
CJ: Yeah, exactly! Anything else to share on Medicare coverage for screening colonoscopies?
Laidy Diana: Well, yes, there's one thing that just like I mentioned earlier about the last year it changed. It also changed that there's another modifier that in this modifier only applied to colonoscopies, high risk or non-risk which are the G0105 or G0121 screening colonoscopies if in our normal FOBT like the fecal occult blood test was, it was termed positive, you have to use KX modifier to indicate that FOBT was positive, was a result, this screening was a result, so the FOBT because prior to January 1st, 2023 there was, if any abnormality of FOBTs, that colonoscopy was no longer a screening colonoscopy for that change, Medicare made that change, and then they say no respire complete colonoscopy screening. The FOBT and that a screening.
CJ: That's good to know. And let me ask you another question, we're getting kind of close to the end of our time together. Tell me a little bit about Medicare handling, billing for anesthesia or moderate sedation during GI procedures.
Laidy Diana: Okay, so when anesthesia or moderate sedation, so if a patient requires an anesthesia, there has to be an indication why a patient requires that, right? So either there was like contraindication just to use modern sedation a patient is obese, they have to really indicate it and it has to be a medical necessity, right? to have the anesthesia in order to be covered for the model that they share, there's some things, some requirements that it needs in order to be billable. And generally, I think last 2017, it happens that now GI procedures can bill with moderate sedation. But there are specific criteria that they need to be made, like for example they need to have a trained observer like maybe an RN who's helping monitoring the conscience of the patient, and then that timing has to be documented. Who administered the sedation and then depending on the payer too, right? So we always go back to who is the payer with Medicare, Medicare that's covered but there's, Medicare create their own G code for moderate sedation, which is the G 0500 which is different than the commercial payers, you know, there's a CPT for moderate sedation, it's 99152. But for Medicare you have to use the G 0500. Medicare does not cover any additional units, like 99153, so it will only cover one unit of G 0500, regardless of how many you can bill them, but it will not be paid and they already pay dollars and pennies on the dollar for that G 0500.
CJ: Exactly! Yeah, I think you're spot on there. Well, this has been really, really helpful information, Laidy. Anything else that before we close anything else on either GI procedures or coding in general or compliance in general that you'd like to share before we close up the recording?
Laidy Diana: I think the only thing I can share with our fellow coders, I think it's always pay attention to documentation when something you're not sure either reach out to someone or reach out to your manager, reach out to your directors or compliance people that you know they can help you and guide you through, I think it's always important to have coding, billing and compliance and the doctors all involved if you're working on a huge organization like the one I work, I think we all come together with something we're trying to develop a policy or anything for our organization. I think it's very important to bring all the people that they're going to be involved in specific codes. So then everyone is aligned. So, I think that's very important.
CJ: I agree, you know, it that transparency and like you mentioned aligning everyone and just so that it's clear for everybody, you get all the and you mentioned you know your prior experience in revenue cycle, it's just making sure everyone's on the same page that everyone understands what the expectations are. If there are disagreements, those are managed, you know, in an appropriate way, as you mentioned you might escalate it up to a compliance committee, but it should be done in a way so that it's clear to everybody. There's nothing worse than, you know, poor communication and a lack of clarity, that's when more mistakes happen. So, I appreciate you saying that.
Laidy Diana: I think you're right. I think transparency you can't be transparency. And I think that's something that I feel like it's important among everyone and all the departments, especially when it makes it harder for big organizations, right? So I think when it comes to like the small practices, it's easier to navigate because sometimes it's one person wearing all hats but aren't huge organizations when they're departmental, and then everyone's trying to do their best. But if you just take the time to come together and say, let's develop this policy and let's, you know, from the coding perspective, from the physician clinical perspective how we can we come together and I can hear the providers point of view from their clinical side and then they can hear what I can say about coding, you know, and how bundling it, it's applied and they might not be aware of those ones. So I think it's very important to be transparent among colleagues.
CJ: I agree and those relationships as you develop them, you know with certain physicians or certain departments that can just help over time. So good advice, Laidy, thank you so much for sharing all of your knowledge and experience.
Laidy Diana: Oh, it is a pleasure! Thank you so much for inviting me to your podcast! I appreciate it. And I hope everyone can benefit from this topic.
CJ: Yes, thank you so much, and thank you to all of our listeners for listening to another episode of Compliance Conversations. Please share these with friends and colleagues if you enjoy them and also reach out to us if you have a topic that you would like covered or if you have a guest, you know somebody, maybe it's yourself, maybe it's a college that you think would make a good guest. Please reach out to us. Thanks, everybody! Take care!