Episode 92:
Telehealth Beyond Borders: Legalities and Logistics
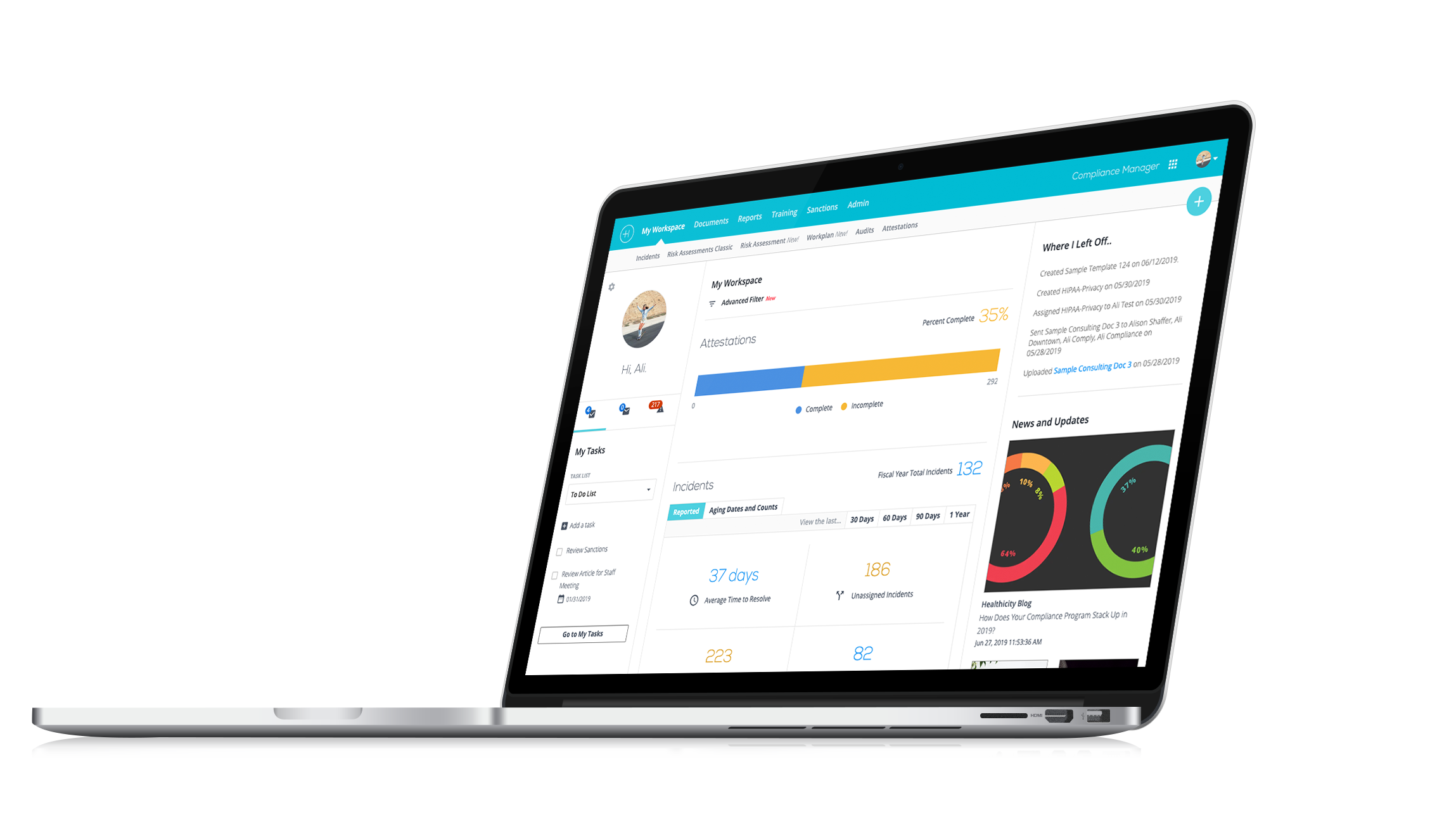
Watch the demo:
Compliance Manager
See the only all-in-one compliance solution today.
Are you intrigued by the rapid evolution of telehealth and its impact across the globe?
Are you intrigued by the rapid evolution of telehealth and its impact across the globe? Then you won’t want to miss our latest podcast episode where Keisha Wilson and CJ Wolf discusses the nuances, challenges, and opportunities in international telehealth services!
In this episode, we discuss:
- COVID-19’s Impact on Telehealth: Learn how the pandemic prompted a reevaluation of international telehealth practices and regulations.
- Compliance and Legalities: Keisha dives into the intricate details of understanding and navigating international laws and compliance issues, ensuring seamless and legal telehealth services across borders.
- Challenges and Solutions: From infrastructure limitations to insurance hurdles, Keisha shares real-world examples and innovative solutions to delivering healthcare to remote and underserved populations.
- Global Collaborations: Get insights into how organizations like the International Society for Telemedicine and eHealth (ISfTeH) and the World Health Organization are shaping the future of telehealth.
- Regulatory Requirements: Understand the various certifications, permits, and legal considerations necessary for practicing telehealth internationally.
Tune in to our latest episode and join us in exploring the dynamic world of international telehealth.
You can also listen to Keisha and CJ’s previous conversation, “The ABCs of ABNs.” CJ and Keisha also mentioned a previous episode titled “Critical Care Anywhere: Exploring Tele-ICU's Impact” featuring Jeni Colarusso.
Keisha Wilson, CCS, CPC, CPCO, CPMA, CRC, CPB, Approved Instructor, is the Founder/CEO of KW Advanced Consulting LLC, Minority Women Own Business Enterprise (M/WBE) Certified, with 20+ years in healthcare specializing in various areas of compliance. Multi-specialty, Telehealth/Telemedicine, Risk Adjustment, provider and coder training. She currently sits on a Board of Directors for an outpatient mental health clinic. Keisha is a licensed PMCC who teaches coders looking to become Certified Risk Adjustment (CRC) and hosts various compliance documentation and coding webinars. She is a published author, having written for AAPC editors on Primary Care Coding Alert, Healthcare Business Monthly, and KW Advanced Consulting coding articles. Keisha can speak at various events this year, including the AAPC Regional Conference on Philidelphia and Cohen's Coding Summit on Telehealth in the U.S. vs Internationally.
Additional Resources:
International Society for Telemedicine & eHealth (ISfTeh): https://www.isfteh.org/
Joint Commission International: https://www.jointcommissioninternational.org/
General Data Protection Regulation (GDPR): https://gdpr-info.eu/
World Health Organization (WHO) Global standard for Telehealth: https://www.who.int/publications/i/item/9789240050464
Interested in being a guest on the show? Email CJ directly here.
Episode Transcript
CJ: Welcome everybody to another episode of Compliance Conversations. I'm CJ Wolf with Healthicity, and today we're going to be talking about telehealth but from a new kind of slant, perspective and we'll share that with you in a moment. But to help us talk about this topic, we are welcoming Keisha Wilson back to the podcast. Welcome back, Keisha!
Keisha: Thank you so much so much, CJ! I'm it's a pleasure to be back!
CJ: But we loved having you on the podcast before, and we're grateful for your expertise in this new area that that we're going to discuss. But before we jump into that topic, maybe you could just kind of refresh our listeners memories on a little bit about yourself. You know, your background, what you're doing now, anything in that regard that you'd like to share?
Keisha: OK, so my name is Keisha Wilson, again, as CJ mentioned, I'm the founder of KW advanced consulting, so I've been in healthcare for over 20 plus years, probably almost touching 30, even though most say I don't sound like it and I've held various positions from front desk, coder, auditor, compliance manager, interim director and then now consulting where I kind of do the same as I did in compliance. I do a lot of reviews and educations for physicians looking to start a practice not sure how, I assist with that from a compliance aspect and then go in and provide a lot of education. And I also teach coding. So, I'm versed in various topics when it comes to coding and telehealth and telemedicine has been one which we will be talking about today and it's even before COVID, I've worked with organizations that was utilizing telehealth and telemedicine. So, I'm excited to be here again today and talking about this one and bringing some examples and expertise from past projects and current projects that I'm working on.
CJ: Perfect! And so, if you're approaching 30 years in the healthcare industry, you must have started when you were like 8 years old!
Keisha: Yes, I like to think about eight or nine!
CJ: Very good! Well, and I love I love your background because you've had positions in so many different chairs, right? Like you mentioned you've seen, you know, from frontline to middle all the way to compliance all these different perspectives so that I think lends a lot to what you bring and as well as what you do to the clients so, excellent. So, I'll spill the beans; telehealth but international, you know, we live in a world today where borders are a little bit more nebulous, people travel more frequently, economies are more tightly, you know, bound together across international borders. People are working, you know, remotely. All of these things are coming together at this time of the world, and our health is important and we've experienced, you know, the boom of telehealth within the United States, especially since COVID. But as you mentioned, there was a lot of being done before COVID too. But we wanted to talk a little bit about telehealth internationally and Keisha has some expertise and experience in this area. So, Keisha, maybe we just begin by just, can you tell us a little bit about how you even just started working with telehealth from an international perspective?
Keisha: Awesome! So, it's funny with the back story, as you mentioned with COVID, a lot of patients were traveling so initially some organization had patients where they were international and wanted to know can they see them? Is it compliant? Are they allowed to? So, a lot of it stemmed from there during COVID kind of researching and understanding international laws when it comes to seeing patients, we know in the United States you had to be within the 50 states if your patient was overseas, you were not able to see them at least within the United States and what they had with the jurisdictions and different stuff like that. But on another level, I have some clients and without you know confidentiality without saying their names, they initially came, they were physicians and they were looking to see patients internationally provide telehealth services and wanted to know if I can assist with research and what does that look like? What does it entail? Are they allowed to do that? Is there any ramifications or any compliance issues with them being in the US and seeing these patients internationally?
So that began my work and it wasn't one day of research, this was weeks and months of research because you know how understanding telehealth in the United States alone is a lot. I've got a lot of worry from that. So, imagine internationally, because it's countries and understanding each country each law, what is going on? It's completely different, so that's how I really got started and I continue to work with them as they continue to unfold and launch. And from that I also got introduced to an organization, the International Society for Telemedicine and E-Health, and they've been around for decades and they are doing a lot of work internationally. And so now that I've met them and took membership, I'm learning even more about telehealth internationally and using my compliance background to assist others, internationally as well. So that's a little back story about how I got started in it.
CJ: Yeah! Well, that sounds like a natural way to get involved in it, right? Physicians or your clients or wherever they may be, you know, asking; "Okay, what happens when we have patients that are international and you know we can still take care of them and still do telehealth." So that's a really good kind of way to set the stage here. So, let's go a little bit deeper then. So, tell us if there are any differences, but then also maybe share some of the similarities regarding telehealth between the US and international countries, there are some differences and similarities.
Keisha: And I would say also with the clients, for example, they noticed and with many when it comes to seeing patients internationally, their goal is more so the disparities and assisting clients in those areas because they may not have access same as the rule health areas in the United States, right? They may not have access to care. For example, like if we think about patients in Africa, sometimes they don't even have transportation to get to certain places. So, there are quite a few physicians and organizations working to help patients where there's children, women, families just get better access to care. And that's why a lot of organizations now are coming together to provide better services to those patients. And so those clients, for example, realized that there was an issue. Patients are spending thousands of dollars to try to get here to see if they can get care. "Hey, we can provide these services with our specialty to these clients. In a compliant manner, once we're able to do so and then getting the government and everyone to back and understand it."
So, I would say that starts the conversation between the US and internationally, there are a lot of similarities where telehealth and both locations have been happening, telehealth, telemedicine for quite some time and we're talking about decades into the early 1900s, but a lot of people did not know, did not understand, right? We all fail for lack of knowledge. So now as time has progressed and COVID-19 came about, everyone's like trying to communicate with their patients, see their patients. And this brought about an awareness with both international and the United States with how can we provide access to our patients and do so compliantly and avoid any risks when it comes to their health.
So that's a lot of similarities that they both have that now the ball has been rolling and they're more aware and they're trying to work together and governments are trying to work with physicians and see what they can do, what platforms are out there.
I would say when it comes to the United States, you know, you have to be within the 50 states. There was a lot of stuff when it comes to cross states; licensure and privacy and what we're allowed to use as platforms to see our patients. Now when you think about international, you know, the United States follows HIPAA and the Privacies, internationally, they follow the GDPR. So, for those that never heard of it and was like, "What is that?" So that's the General Data Protection Regulation and some call it GDPL; Law. And that's the data privacy when it comes to seeing patients internationally when it comes to the European countries, but when you think about it, a lot of the Caribbean and other stuff falls under the EU.
So, they say the GDPR is one of the strictest data privacy laws. And even the United States, a lot of organizations use some part of the GDPR because it's still strict when it comes to data privacy and transferring data. So, when you're thinking about international, you have to understand the laws of each country. Are they following this? What is the privacy or their ramifications when it comes to breaches? Who do you have to talk to? Is there laws? Not all countries have laws yet when it comes to telehealth, because again, it's still new for a lot others that has been using it since the early 2000s have laws updated their laws recently to make it more strict when it comes to privacy and patient data and so that's what you're seeing a lot now.
Africa again, for example, Australia has similarities within the US where they also have like a Medicare where for example, you had to have a relationship with your provider before you use telehealth with the patient, but with COVID, they kind of relaxed a lot of stuff. But again, now they're going back to those you had to have an established relationship. So, when I was researching, I was like; “Oh, this sounds a lot like the US,” so there's a lot of similarities, but there's a lot of differences where you may not need to use a specific platform because this country may not have strict laws, but others that have strict laws, you have to be very careful. And what I notice is that there are a lot of companies now internationally that are creating platforms, compliant platform. And then the government to trying to get behind it, to understand it and back it and that's where you want the support.
CJ: That makes a lot of sense, you know, and also just your beginning statement talking about bringing top notch healthcare to people who just don't normally have access, right? They can travel or more rural, that one of our prior podcast episodes, we talked about kind of this equity and some of the beauty of telehealth is bringing medical specialties and expertise to people who 30 years ago would have to have traveled to see that individual in person. So that's kind of the beauty of it. So, I like that as kind of one of these similarities, it's kind of driving telehealth. And I'm also glad you mentioned the GDPR, you know in some work I do with clients too, even outside of telehealth, GDPR is for any data, right?
Keisha: Yes!
CJ: But a lot of data that deals with the EU, the European Union and there are a lot of U.S. companies. And this GDPR will apply even if you're not stepping foot in Europe, but if you're exchanging data from Europe, so there's GDPR is, I'm glad you mentioned it that's a good one for people to kind of think about and look into. So, with all of that said, kind of differences and similarities, do you have or maybe you already have shared a specific example of a challenge or opportunity that are presented by those differences? Do you feel like you've already addressed that?
Keisha: And I'm glad that you touched the GDPR again, because that was one, I would say bump in the road that came across doing a lot of research is EHRs and EMRs, because of that data, as you said, transferring of that data internationally it creates like a lot of, people like; "Oh my gosh, you know, I don't want to deal with this." So, there's a lot of companies who have great platforms here in the United States but when you talk to them and say; "Hey, I'm looking to see patients internationally," they're like; "Nope, we're not doing this." You may not even get a call back because they understand the ramification of seeing patients internationally and if there is a breach, what can happen and not everyone may necessarily want to deal with that. So now it's finding the right platform where you can keep your patient data, store it appropriately, make sure you're checking all the marks when it comes to privacy, and making sure your patients understand that.
So, I find that getting to work with the vendors, you may think that; "Oh yes, I'm working with this vendor in the United States and they'll work with you when you're seeing patients internationally." And that's not necessarily a part of it, so that would be one bump.
The other one is insurance companies internationally, just like the United States, not all insurance companies cover telehealth or telemedicine. They did it before, some still don't know. Some also require you to be on the ground in order to provide this service to your patients. So, you come across or you have an issue where it's not necessarily covered by the insurance company. Can your patients afford this service and if not, do they have some type of government program that will assist the patients because some of them have real conditions that need to be addressed right away, so then if not you as a doctor, what are you going to do?
Another thing I would say with the issue is broadband, you know, really getting access to these patients, because of the locations and area they're in, so the infrastructure, so now you have a lot of governments initially they were run by said they weren't interested or they just didn't understand but now with COVID, they see the need so they're working with those and they're trying to see how they can build up so that providers, if they're not within those countries can communicate with those other patients. And physicians are using it too. They were actually the ones that was using it initially to like E-consult, almost communicating with each other for second opinions about patients.
CJ: Right!
Keisha: So, I definitely say the vendors understanding the insurance and then also you have the money, right? Each country's currency is a little different, so you may have this mindset with how Medicare and private payers here in the United States pay, but it's completely different over and especially when you think about the currency, you can't necessarily or you wouldn't charge a patient. How you charge them here in the United States, you may not charge them there. So then trying to come up with an appropriate, like fee schedule of how you're going to charge these patients, especially some of them can't afford it.
CJ: Yeah, those are all great examples. This is really a great conversation! We're going to take a quick break though, and we're going to come back and continue talking about some of these telehealth issues as it relates to international telehealth services. So, we'll be right back in a moment.
Welcome back everybody from break! We are talking to Keisha Wilson about telehealth internationally, and Keisha we were talking about, you know, you shared some really good examples, and I wanted to provide one before we get to the next question or kind of comment on one that you shared, you just talk about broadband and infrastructure. I'm involved in in higher education and I'm involved in an institution where we're bringing education to students worldwide, this is a religious institution, and trying to provide education that started in the US and transformed those classes into classes, college classes that are appropriate for international students, like in Africa and Southeast Asia, South America, and one of the biggest issues is designing classes that don't take a lot of bandwidth, right? Because just as you mentioned, we all take our phones for granted, right? We think; “Oh I can talk to a doctor if I need to,” but in many places of the world it's either not accessible or it's expensive, right? So, it's really expensive on the data from a data standpoint to, you know, to use a lot of your cell service data. So, I'm glad you brought that up as one of your examples.
So, if we could move on a little bit. So, tell us about what are the countries legal and regulatory requirements for telehealth services? Things like, are there specific licenses needed, permits, certifications, that are that are needed to be obtained to have a practice telehealth overseas? And are there any organizations that might assist those who are interested in going to this next step of implementing this type of service?
Keisha: And I like how you mentioned about the higher education and taking it outside the US and I think now a lot of organizations are doing that or looking to do that because when you think about it, we have a lot of international students as well. And so, they're coming back. So, having them understand telehealth and telemedicine and the impact we're moving from educating physicians from bedside to web side, right?
CJ: Yeah!
Keisha: Website manner where you still want to provide this top-notch service to your patients, even though you're doing so from a distance,
CJ: Yes!
Keisha: A lot of organizations are working around that to say; "Hey, we need to implement this as well with education, how do you really talk to a patient the same way you would in person, but now with the web?"
So, I see a lot of organizations creating programs. Some are creating accreditation programs, so I don't know if everyone's familiar with the Joint Commission here in the US and we know everyone always gets nervous when they come to the hospitals.
CJ: Right!
Keisha: Everyone sweat and stress, but they also have a Joint Commission international now a lot of people don't know that and they have accreditation programs and they're working with over, I think, 70 plus countries. And they're working with hospitals and clinics and physicians to get them a credit to say; "Hey, we're providing this kind of quality care to the patients, even though they're international, like we're not treating it very different." And I think that's amazing.
I know the World Health Organization is also teaming up with the society I mentioned before, ISfTeH, they're working with them to provide a lot of education to countries so that they understand what it takes to really see the patients and do so compliantly.
So, when you're seeing patients internationally, you really have to look at each one you can't assume and research, you can't just go to one page and think that that's it. You really have to take a deep dive into those countries, look at their laws, their privacy laws, a lot of them have privacy laws and we think; "Oh, yes, maybe they're a small country and they don't," but they're, they do where they want to know if there was a breach within 48 to 72 hours. You do have to get certified or you have to be board certified or registered in those countries as well.
So, the clients I mentioned, for example, the countries that they're going to be working in and seeing patients in, they went physically to those countries and got certified with them and they had to provide their information from here as well. So, it's not a simple process. There are certifications you have to get on the insurances. Malpractice is important. So, you do have to take out malpractice insurance. Again, you're seeing patients internationally. So, I would say you have to look into that. You want to get a health care lawyer that understands international, seeing patients internationally, on what that entails to also make sure if you're seeing patients here that doesn't conflict with any contract that you may hold with the organization here as well.
CJ: Good point!
Keisha: So, malpractice, we have board certified. You also have, as I mentioned, the Joint Commission, so there's a lot of places or companies now that's coming out with accreditations to show that; "Hey, we're backing these providers, these organizations, to provide high quality care to these patients." And I think that's great. I really see the progress, especially in doing the research and I really would say that COVID-19 really like catapulted everyone to kind of move faster. Even in Saudi Arabia like they're big with a lot of platforms and they're getting a lot of backing now with like Joint Commission and who because they see the need and they see the disparities and they want to help these patients.
CJ: Yeah, well, that's really helpful to understand Joint Commission's role internationally, what they're doing at the World Health Organization and then the society that you've mentioned a couple of times, I think you said it's the ISfTeH?
Keisha: Yeah!
CJ: If that's right, maybe we can have you send us that link and we can include that in the show notes as well that might be helpful.
Keisha: Oh, yes, yes. I actually went to a conference in San Jose, CA in December and it was so interesting, like I was doing one part of the research for the clients and then all of a sudden, you know, social media comes up and I'm like; "Oh! There's the International Society that's having a conference for like a few days, I should go." And it was so impactful because they had so much people there, and you're learning so much about international as well as the US, right? They had the American Health Association there. They had CCHP there as well. And so, it's really understanding telehealth and educating those with what does it look like internationally. And everyone's main focus is patience and providing better quality care, and I like that and I like that about them and other organizations as well.
CJ: And that's great, thanks for sharing that! So, let me ask you this getting into maybe some more of the challenges you know in your experience, what are some of the main challenges associated with delivering telehealth services in countries that have this limited access to technology, or to reliable Internet infrastructure, right? We talked a little bit about it. Do you have anything more to say on that particular point?
Keisha: Yes! So, I would say you definitely have to look at the country in particular, what the infrastructure looks like. The government, what are their policies? Are they looking to team up and update? You know, oftentimes its funding is an issue and then if not, what are you going to do? So, I know for some of the eastern Caribbean countries, that was definitely an issue.
CJ: Sure!
Keisha: So, thinking about if the patients are up in the country and they don't have access to internet, you know, how are you going to provide this service. And I see a lot of organizations or thinking outside the box where maybe if there's a place, or an office in town for example, or a local city that has, you know, busting those patients in maybe once a week and this is where they like a clinic and this is where they're going to provide this telehealth service or telemedicine service to this patient because from their homes, they won't necessarily have access, but from this location, they will. So, in the interim, while they're working on infrastructure, I see this is what's happening. There're different clinics popping up that has access and this way they can communicate with their patients.
So, I definitely feel like infrastructure is a big thing. Sometimes some governments may feel like; "Well, this is a lot more than we expected." So, you really have to put together a proposal when you're pitching to this country to say; "Why do we want to provide this service? What is the benefit?" Sometimes, you know, it's just life. They want to know what is the benefit for us if we go into this, you know? And provide this service and give you the funding to do this. How long is it going to take? When are we going to see our return? And so, kind of getting them to understand and sometimes you just have to show data, right? Some people love data, so you have to show them examples from other countries and what are they doing.
I think Jamaica for example now is doing like they have a great pilot that's been happening since 2018. They updated their standard; they're providing telehealth to their patients. And we're thinking and I just like what they're doing. They have like a whole PDF together with what they can provide, "Yes, you can use tell- audio only. No, you can't use it. Do you have to have established patient relationship? You know what happens with connectivity."
So I think everyone's learning and growing and evolving. And then you also have these positions, who are older and younger, working together to really come together and provide the service because they see a need.
CJ: Yeah! I think that's really the main point, right? Is the need and that is driving kind of this whole work is that so much can potentially be accomplished through this, right? Bringing the information and bringing the brain power of the medical world to people instead of requiring them to physically come. Now, of course, after the surgery or something, right, you got to be there in person. But a lot of healthcare, especially preventative medicine can be done through these other communication lines, and then you can monitor people, right? Like let's say you've got somebody who is diabetic, or they got heart disease and you've got them under control rather than requiring them to take a bus ride for three or four hours, you know, once a month, maybe you can do some of that monitoring, interviewing remotely, saving resources, but also still giving excellent care. So, I think it's really promising too. I can tell in your voice that the excitement that's there for the countries that have not always had these opportunities, that's exciting.
Keisha: Yes, yes. And even in maternal health, you know, I see that big a focus with monitoring and as you mentioned, it's not just communicating with the physician but monitoring their health, to see the moms and babies through delivery and safe delivery and I feel like the telemedicine and telehealth has opened a window where they can provide better health in these countries to these patients. You just have to find a way to do so compliantly and work with the government when it comes to infrastructure.
CJ: Yeah, exactly! So, you you've mentioned already a little bit about you know assessing you know that countries insurance and reimbursement policies, right? A lot of countries have a kind of a nationalized healthcare system. But tell us a little bit more about what you know about reimbursement or payment for telehealth services in countries overseas, so maybe patients use government healthcare programs, do some use private insurance or some doing out of pocket payment options. What can you tell us about that general topic?
Keisha: So, there's, I would say there's a little bit of both depending on the country. So, Australia for example has similar like Medicare, where they cover for the government, for those that fall under that umbrella. And then there's a lot of private insurance as well. And you find it in a lot of the established countries, the smaller maybe Caribbean islands they do have insurance, private insurance, they may not have like a big one like Medicare, but they do have private ones.
So, some, just like the United States, did not cover telehealth or telemedicine at all initially, but they do, depending on a limited basis, right? What you can communicate with. So, they may also have where you need to have an established patient relationship, or you can only use audio and visual similar to the United States. Others it's a little more relaxed, so it depends. It also depends where is the physician located. I will also say that some private insurance coverage, some don't. So, you see a lot of patients paying out of pocket for the service because they feel like it might be cheaper than getting on a flight, we can't afford that. So, they may come together, they may raise funds as a community because this person is diagnosed with this certain type of condition. And so, they go out together, they raise money so this patient can now get access to care.
So, I see that a lot in some of the countries, if they're not paying for their patients, will pay out of pocket or they would be some type of funding to allow this patient to do it. So, they don't always have, you know, here in the United States, there is something if a patient is having hardship.
CJ: Right!
Keisha: Other countries may not have such a thing, so now it's like thinking outside the box of how are we going to provide this service? But I think a lot of insurance companies and I've had meetings with at least three. And it's always interesting they're willing, they're looking, you know, COVID opened their eyes as they would say, to covering it. And so, you can submit claims how you submit claims is a little different. Not everyone may be online, so some you may still be doing a lot of manual labor or you're faxing and e-mailing stuff to them and waiting for approval. Some patients may have to pay out of pocket first. And then you have to give them all the receipts and claims and they submit that to the insurance company and they would be reimbursed. They may not be reimbursed for everything because some feel that you can either see the positions in the country, if not some have where you can see them within the surrounding area.
CJ: Right!
Keisha: So, they giving you a few options, countries surrounding areas before you go out and see a physician. So, if you just chose to go out and see one out of the country and out of the areas, they may not cover it at all, so it's important for the patients to communicate with their insurance before they see a physician that's not located in that country. So, it's really interesting when you speak to the insurance companies, it's similar to us, but it's also interesting and they a lot of them have a physician-based referral.
CJ: Right!
Keisha: So, they want the patient to be referred to you from a primary care. So, there's a lot of networking that providers have to do in order to see patients, you may need to go on the ground and explain that this is not a competition, but we're working together for the better health of the patients and when they have the referral in the system, they may be more likely to cover it.
CJ: Yeah, that's really good information, Keisha. This has been fascinating. We're getting kind of towards the end of our time here, and I want to, if you have any last-minute thoughts or comments or hopes or you know where you might see this going. If you're going to try to predict the future a little bit. Do you have any last-minute thoughts on any of this before we wrap up today?
Keisha: I would say that I'm excited to see Telehealth and Telemedicine grow internationally, as well as the US. I think each is looking back and forth at each other to see what they're doing. And last but not least, Alaska has been doing telehealth for quite some time, more than the other states in the United States. So, it's interesting that we are now looking to Alaska to see how did they do, you know, how could we do better? So, I think we can all learn from each other to provide better care to our patients.
I'm looking forward to continuing to educate, you know, and provide information to people, but I think once we keep our patients in mind and just educate and understand what's out there and how can we help and you know, I think we just seem to be beginning of telemedicine and telehealth when it comes to international.
CJ: I think you're right. And I think it's just, it's going to grow and I just think in my lifetime I look back I'm like; "Whoa, we never used to do that. And look at what we're doing now." And so, if I can live another 20 years, 30 years, whatever, what's going to, you know, we're going to be able to look back and be like; "Wow, we talked about this 20 years ago. We talked about this thirty years ago. Look at what's happening now." So, it's exciting!
Keisha: Exactly!
CJ: Thank you so much, Keisha, for sharing your time and your experiences on this particular topic. Thank you all for listening to another episode of Compliance Conversations. Please share these episodes with friends. Subscribe, spread the word, and if you have topics that you want address, please reach out to us. And if you know of speakers or people who have expertise like Keisha in many different areas or certain areas, please recommend them to us and we can explore maybe getting them on the show as well. So, with that said, thank you all for listening and have a great day!